

Volume 11, No. 1, Art. 7 – January 2010
Through the Looking Glass: Public and Professional Perspectives on Patient-centred Professionalism in Modern-day Community Pharmacy
Frances Rapport, Marcus A. Doel, Hayley A. Hutchings, Gabi S. Jerzembek, Dai N. John, Paul Wainwright, Christine Dobbs, Stephen Newbury & Carol Trower
Abstract: This paper presents five consultation workshops with 29 community pharmacists, stakeholders and patients that examined "patient-centred professionalism" in terms of pharmacists' working day and environment. The concept is ill-defined in both medical and pharmacy literature and the study aimed to clarify the situated nature of the term for patients and health professionals across settings. Workshops were supported by bio-photographic datasets of "in-situ" practice and Nominal Group Work.
The thematic content analyses led to the following aspects: building caring relationships; managing external forces; the effects of space and environment, and different roles and expectations. The study reveals how patient-centred professionalism cannot be defined in any singular or stationary sense, but should be seen as a "moveable feast", best understood through everyday examples of practice and interaction, in relation to whose experience is being expressed, and whose needs considered. The phrase is being mobilised by a whole set of interests and stakeholders to reshape practice, the effect of which remains both uncertain and contested. Whilst patients prioritise a quick and efficient dispensing service from knowledgeable pharmacists, pharmacists rail against increasing public demands and overtly formalised consultations that take them away from the dispensary where the defining aspects of their professionalism lie.
Key words: patient-centred professionalism; UK community pharmacy; public and professional perspectives; bio-photographic data; consultation workshops
Table of Contents
1. Rationale
3. Background on Community Pharmacy Practice
4. Study Aim
5. Method
5.1 Recruitment and sampling
5.2 Consultation workshops
6. Analysis
7. Findings
7.1 Demographics of five consultation workshops (Session 1)
7.2 Patient-centred professionalism—thematic findings
8. Conclusions
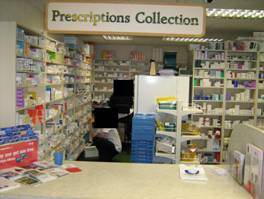
Appendix: Bio-photographic Material from UK Community Pharmacy
This paper reports on a study using extended consultation workshops with a range of health professionals and patients1) in Wales, UK, to gain a greater understanding of the concept "patient-centred professionalism" in modern-day community pharmacy. The study aimed to clarify what patient-centred professionalism meant to different groups of people in the context of the pharmacist's working day and work environment. Understanding was enriched with bio-photographic data contextualising the study and offering examples of the "in-situ" nature of practice in different work environments, utilised from two previous studies of general practitioner (GP) and community pharmacy settings (RAPPORT, DOEL, ELWYN & GREAVES, 2006; RAPPORT, DOEL & ELWYN, 2007; RAPPORT, DOEL & WAINWRIGHT, 2008a; RAPPORT, DOEL & JERZEMBEK, 2008b). [1]
2. Patient-centred Professionalism
The pharmacy literature provides little insight into the concept patient-centred professionalism in the community, despite renewed interest in the topic (DROEGE, 2003; WILLIAMS, 2007; PHARMACY PRACTICE RESEARCH TRUST, 2009). The broader healthcare and medical literature describes patient-centred professionalism as central to a vision of healthcare evolving appropriately within society (BOHM, 2004; PICKER INSTITUTE, 2008). This includes instilling good professional values and standards at an early stage in professionals' training and ensuring greater awareness of patient safety issues, in line with a clear professional Code of Ethics (GORDON, 2003; ROYAL PHARMACEUTICAL SOCIETY OF GREAT BRITAIN, 2007a). Dame Janet SMITH commented that enhancing knowledge and skills takes place during career development, but fundamental to that, are professional ethical standards and attitudes which must be instilled during training (GENERAL MEDICAL COUNCIL, 2005). However, there has been little guidance on how to instil such attitudes and, more fundamentally, what the notion might mean to health professionals and patients, despite the wide variety of definitions that abound (see for example: EPSTEIN & HUNDERT, 2002; ROYAL PHARMACEUTICAL SOCIETY OF GREAT BRITAIN, 2007b). Ronald EPSTEIN and Edward HUNDERT (2002) suggest the notion is predicated on a range of professional and technical competencies, including communication, knowledge, technical skill, emotionality and clinical reasoning. [2]
The study we describe in this paper was based on the premise that to nurture positive professional values and practices, through well-designed teaching and learning initiatives to create the key pharmacy leaders of the future, one must first understand the notion "patient-centred professionalism" more clearly. This can be achieved by close observation of professionals in the workplace or, as in this study, through in-depth discussion with patients and professionals to clarify what influences people's understanding. We undertook workshops with: pharmacists (both experienced and newly registered), stakeholders (lecturers, policy developers and implementers), pharmacy staff and the public, to understand how the concept affected personal function, working practice, skill development and formal and informal communication. Pharmacists and pharmacy staff were chosen to represent a range of community pharmacy settings and environments from small independent shops through to large specialist stores and pharmacies in multi-national supermarket outlets. [3]
3. Background on Community Pharmacy Practice
Community pharmacy in England and Wales has undergone considerable change in recent years resulting from the new National Health Service (NHS) contract and policy framework for service provision (DEPARTMENT OF HEALTH, 2005; WELSH ASSEMBLY GOVERNMENT, 2005). The framework included a new, three-tiered community pharmacy service, comprising essential, advanced and enhanced services. Essential services included medicine dispensing, and promotion of healthy lifestyles. Advanced services included Medicine Use Reviews (MURs) (how patients use their medication), and prescription intervention services. Enhanced services included smoking cessation programmes and supplementary prescribing, such as emergency contraception. The new services enabled some pharmacists to qualify as supplementary or independent prescribers to help broaden services, increase pharmacists' availability and accessibility and promote healthcare within the community (DEPARTMENT OF HEALTH, 2008). [4]
As a result, consultation rooms were brought into all community pharmacies for confidential discussion and pharmacists began to have timetabled consultations with the public (BLENKINSOPP, TANN, EVANS & GRIME, 2008; DEPARTMENT OF HEALTH, 2005, 2008). According to Hannah PIKE (2007) however, whilst consultation rooms increased sales of specific items such as incontinence products, they also reduced the pharmacy floor space, and, consequently, income from retail sales. Alison BLENKINSOPP and colleagues 2007 survey, commissioned by the PHARMACY PRACTICE RESEARCH TRUST (BLENKINSOPP, BOND, CELINO, INACH & GRAY, 2007), indicated that the new contract also increased workload and raised issues about delegation of tasks to staff. Pharmacists were said to be uncertain about how much information to share with members of the public and, with lack of clarity about the specific components of advanced or enhanced service, reluctant to offer services widely. Furthermore, whilst direct contact continued to intensify, there was little clarity about the nature of interaction, which had previously fallen within a professional dominance model (SKOGLUND, ISACSON & KJELLGREN, 2003). [5]
In view of these changes and their reported impact, this study aimed to:
Clarify situated understanding of patient-centred professionalism across a range of settings;
Position the knowledge in a modern-day environment, accessing the opinions and experiences of patients and professionals;
Inform the literature on the value of consultation workshops within the community care context. [6]
The study was conducted in two phases: Phase I involved half-day consultation workshops with community pharmacists (all seniorities), pharmacy staff, patients and pharmacy stakeholders. Following collation and organisation of those datasets and individual and group analyses, Phase II expanded and refined definitions of patient-centred professionalism through coordinated feedback and data gathering workshops with newly qualified pharmacists. Each workshop was tri-sessional, but this paper reports the outcomes of Phase I, Session 1 only, to convey the distinctiveness and richness of Session 1 data. Whilst we cannot elaborate on all aspects of the workshop, we would emphasise that this nevertheless upholds the aims expressed in Section 4, indicating the multi-professional nature of the consultation, the involvement of members of the public, thus widespread views, the in-depth nature of consultation workshops and their value within a community care context. [7]
Pharmacists and pharmacy staff were recruited through a purposive sampling approach (QUINN PATTON, 1990) according to the full range of community pharmacy types from independent pharmacies to large chains including those in supermarket stores. The team (see author list) had already made extensive links within the local communities in South and Mid-West Wales and added to these through local stakeholder meetings and Local Health Board (LHB) lists of pharmacists registered across regions. By concentrating on community pharmacists rather than hospital pharmacists who practice in environments with completely different dynamics, the team could ensure that those most isolated in practice and less supported by their peers and other healthcare professionals were involved. Similarly, the sample included pharmacy locums (temporarily fulfilling the duties of a pharmacist), who frequently work across settings with different professionals. [8]
Patients were recruited across regions purposively, to ensure a breadth of views including those of: frequent and infrequent users, the elderly and teenagers, carers, long-term illness sufferers and parents of young children. Patients were recruited through pharmacy contacts, Expert Patient Panels, team contacts and by word-of-mouth using snowballing techniques. [9]
Stakeholders were recruited across the regions with the support of LHB lists and contacts with major pharmacy companies. Stakeholders represented: lecturers and educators, major pharmacy and regulatory bodies, policy developers and implementers. [10]
Once identified, potential participants were sent information packs, defining the study and explaining about data confidentiality and anonymity, and consent forms, which they signed and returned to indicate willingness to participate. Participants agreed to notes being taken and workshops being tape recorded. [11]
Consultation workshops are facilitated, extended group interactions comprising small group work and individual activity. Facilitators provide direction and advice and often work together to enable multiple activities to take place (CHAPPLE & MURPHY, 1996). Facilitators pay close attention to group dynamics and group cohesion, the way conversations develop across sessions and how complex tasks follow on from each other. The group's response may be considered "cumulative", as one session influences the next and leads to a deeper clarity of understanding (CLAXTON, RICHIE & ZAICHKOWSKY, 1980). [12]
In line with the literature (CHAPPLE & MURPHY, 1996; BLOOR, FRANKLAND, THOMAS & STEWART, 2001), we aimed for an optimal sample of six participants to each tri-sessional workshop. Workshops lasted for approximately four hours. Session 1 examined the "in-situ" nature of community pharmacy practice in relation to patient-centred professionalism. This session was supported by visual and textual data (see Appendix) from two previous studies of professionalism in practice (GP and community pharmacy settings; RAPPORT et al., 2006; RAPPORT et al., 2007; RAPPORT et al., 2008a; RAPPORT et al., 2008b). Session 2 elicited storied examples of working within, or being supported by, community pharmacy, and led to lists of competencies and other elements necessary for optimal patient-centred professionalism. These were refined during Session 3 through Nominal Group Work (DELBECQ, VAN DE VEN & GUSTAFSON, 1975; CHAPPLE & MURPHY, 1996; LLOYD-JONES, FOWELL & BLIGH, 2002), where aspects of positive and challenging patient-centred professionalism were identified, discussed, listed and ranked, to arrive at a consensus of opinion about the essential character of the concept (this work will be reported elsewhere). All consultation workshops were organised and run by the same facilitators (RAPPORT, HUTCHINGS, DOEL, DOBBS) to ensure consistent working practice. All workshops were designed to provide a final list of ten2) positive and ten challenging aspects for consideration by newly qualified pharmacists, refined into Continuing Professional Development (CPD) materials. This part of the study is ongoing. [13]
5.2.1 Session 1 Phase I: Data gathering
In line with the literature (KEARNS, 1991; RADLEY & TAYLOR, 2003), anonymised, bio-photographic datasets reflecting GP's and community pharmacists' own views and images of their workspace, were sent to participants to ground their views and contextualise their experience. Participants were asked to reflect upon the datasets before the workshops, considering their content and implications, and the situated nature of practice. The briefing was left purposefully broad to reduce researcher intervention (ROSE, 2000). Participants were told that datasets were there to stimulate lively, informed conversation, rather than as an end in themselves. [14]
Session 1 was facilitated by one team member two others taking notes and observing interaction. A fourth member recorded the event. The session followed a general introduction that included some "rules of engagement", one person to speak at a time, respecting one another's point of view, and positively critiquing one another's ideas. The group was given the opportunity to add their own rules to the list, and asked whether they objected to being taped. It is interesting to note that none of the groups wished to make any additions. [15]
Session 1 commenced with a lengthy discussion of workspace and practice stimulated by the datasets leading to more directed questions around the nature of patient-centred professionalism in different community healthcare environments. Participants were asked who might work in such spaces, according to a brief interview schedule comprising topic areas: people in spaces, roles and responsibilities, professional identity, development of trust, inter-professional aspect, and talked about the visualisation of space and the ability of photographs to extend verbal understanding. They discussed roles and responsibilities, what it meant to be a professional, how trust was developed, shared and individual tasks, different aspects of practice and differences between GP and community pharmacy workspace. Participants discussed qualities of patient-centred professionalism and how these were evoked. Participants provided examples of their own work and competencies, changes in their practice and their experience of entering a pharmacy as a member of the public or a professional. [16]
Consistent with our previous research, analysis was conducted at two levels, individually and as a group. Using thematic content analysis we searched for initial themes and categories (ROBSON, 2002). These were identified and listed before the research team came together on two occasions to discuss them in more detail and examine defining elements of the session. Workshop facilitators made copious notes during and after the event and these supported the analysis and informed two further meetings with the wider study team to refine the data into clearer themes and categories. Individuals organised themes into schematic frames of reference, and, like grounded theory work, clarified interrelated concepts (STRAUSS & CORBIN, 1998). [17]
Thematic analysis, which has been described as including flexibility of method and purpose (BRAUN & CLARKE, 2006), emphasises the relationship between theme and research question and the ability of themes to encapsulate essential elements of the data which would otherwise lose their full coherence. Whilst there are different ways of indicating the prevalence of a theme without quantification, this study used an inductive method which has been used extensively by other qualitative researchers (see for example: POPE, ZIEBLAND & MAYS, 2000). Inductive methods allow people's views of a text and their interpretation of the text’s meaning to emerge through data-driven discussion and in-depth interpretation. People work together to hone down categories and expand others, to reveal overall surface meaning (semantic meaning) and underlying notions of understanding (latent meaning) (BRAUN & CLARKE, 2006). The process is iterative, beginning when data are first collected and ending after the final dataset have been collected. Significant statements are clarified through detailed example (including verbatim quotation), and patterns of meaning and outlier positions are disclosed. [18]
7.1 Demographics of five consultation workshops (Session 1)
Twenty-nine participants took place in five consultation workshops. Participants were spread across Mid and West Wales regions, across urban and rural communities and groups included both men and women. [19]
The public group comprised six people, four female and two male: two retired women, one a former teacher who described herself as taking a lot of pills and the other with a heart complaint who was a frequent pharmacy user, a woman with two small children also a frequent pharmacy user, a middle aged woman not currently in employment who was an infrequent pharmacy user, a young male law student who had asthma and regularly visited the pharmacy and a male carer who was a regular visitor. [20]
The stakeholder group comprised five people, two male and three female: a head of pharmacy for one of the LHBs, a representative of a professional education body, a policy advisor, a pharmacy board member and a pharmacy lecturer. [21]
Pharmacist group 1 comprised five people, three male and two female: a locum, a pharmacy manager who had worked in the same chain of pharmacies for twenty years, a pharmacy manager who had previously worked with a number of nursing homes, a manager from a pharmacy in a large supermarket chain and a pharmacy manager who had been qualified for three years. [22]
Pharmacist group 2 comprised nine people, six female and three male: spread evenly across different community pharmacy types including those in large supermarket chains and smaller national chains. This group included two locums. [23]
The pharmacy staff group comprised four people, two of whom worked for large pharmacy chains and two of whom worked for smaller pharmacy chains. The participants were spread across Mid and West Wales regions, and across urban and rural communities. [24]
7.2 Patient-centred professionalism—thematic findings
Findings are presented according to the major themes that support or hinder community pharmacists from taking a patient-centred professionalism approach in their work, to shed light on the issues that define a contextualised understanding of the concept for these groups. Quotations are presented according to each group's name, followed by group and participant number (allocated as participants were recruited into the study, for example: patient 1/5, pharmacist 1/4, pharmacist 2/4). [25]
7.2.1 Patient-centred professionalism—building caring relationships
One of the most striking aspects of the pharmacist and pharmacy staff sessions was the notion of pride expressed—in upholding professional standards, managing work and caring appropriately for the public, and wanting to provide them with an excellent service. For pharmacists, the caring role was synonymous with a strongly individualised understanding of what it means to be a professional and, at the same time, a belief in one's own competency. However, by caring, pharmacists saw themselves as "victims of our own success" (pharmacist 2/1). By being so open and accessible they were too much in demand leaving them feeling anxious and put upon by patients who had unrealistic expectations of the services they could deliver. Consequently, whilst pharmacists wanted to be available: "accessibility is our greatest asset" (pharmacist 2/1) and delegate tasks wherever possible, they felt they were loosing control of the overall function of the pharmacy, and found it progressively difficult to achieve balance in their jobs. [26]
Pharmacists recognised the need for good quality "quiet time" (pharmacist 2/3) with patients, to work with them to ascertain their expectations and ensure the minimum MUR requirements were fulfilled to the correct standard. They were also aware that patients prioritised accurate and speedy medication dispensing over all else, and that this aspect of their work was what was most appreciated. According to pharmacists and stakeholders, until the introduction of the new pharmacy contract, dispensing and informal discussion around drug regimes had ensured strong relationships, built gradually over time, through trust and respect: "advice-giving builds up a relationship" (stakeholder 1/2). Pharmacists in particular were keen to stress that they still considered dispensing the mainstay of their job. Trust was linked to "getting dispensing out of the dispensary" (pharmacist 2/7). This was supported by patients, who said: "the pharmacist's primary objective should be to dispense" (patient 1/1). [27]
However, under the new NHS contract conflicting demands mean pharmacists have to spend more time consulting. The problem of how best to change their outlook and divide time more appropriately concerns them greatly. Whilst they wish to continue to work in a familiar and comfortable way, they are aware of the new demands for consultation that they see as taking time away from enhancing technical skills towards formal patient interactions that have to be logged and assessed on a weekly basis. It has also been impressed upon those working for large companies that they must be more visible in their work. Consequently, many companies have changed the look of the workspace, introducing open-plan areas and glass consultation booths. Whilst this brings financial benefits, it also places pharmacists in less-familiar territory, and raises their workload. Tasks have also become more complex, and it takes them longer to conduct a consultation in a booth. Ironically, visibility has to their mind detracted from the public's perception of their competency: "they think it is less professional because you are on view" (pharmacist 1/3), and: "you can't give your full concentration to the job" (pharmacists 1/4). One of the long-standing pharmacists summed it up thus:
"The job has changed dramatically over the last five to ten years. We now have more diversity of role. Before we were just dispensing. We could speak to people and we were not under so much pressure. We are now expected to do MURs and our increase in workload is reflected in the number of tasks we now undertake. There is, amongst the older generation of pharmacists, resistance to change. It is ingrained in many of us that the essential element of our role is to dispense" (pharmacist 2/2), [28]
However, whilst pharmacy staff discussed the need to support pharmacists during this period of change—"I am an Accredited Checking Technician (ACT), trying to take pressure off the pharmacist" (pharmacy staff 1/2)—opportunities to delegate were considered limited. This was due in part to pharmacists' uncertainty about staffs' ability to manage all aspects of the workload and pharmacists' sense of overall (and especially legal) responsibility: "we remain can-carriers" (pharmacist 2/1). It also reflected the external pressures of stringent new policy regulation and Government targets (see Section 7.2.2 on "managing external forces"). Pharmacists repeatedly described themselves as "anxious" and "demoralised" (pharmacist 1/3), disliking the new administrative aspects of their job:
"if you choose to work for a particular company you have to abide by their rules, but there is a lack of support. You have to give time up to devote to issues like payroll. This is constant and takes you away from professionalism" (pharmacist 1/2). [29]
Consequently, many pharmacists have changed jobs to become locums, or part-time pharmacists, to alleviate administrative responsibilities.
|
"We need to speak to patients, but we may not have the time" (pharmacist 2/9). "[Whilst] dispensing a prescription, customers may call over. The prescription is then waiting, the train of thought is interrupted" (pharmacy staff 1/4). "We have to do everything. We are getting spread thinner and thinner" (pharmacist 2/2). "I hate it from the patient perspective. I always go to see a patient if they want something, but they must see the annoyance on my face if I am busy. I shouldn't have to pass that feeling on to them" (pharmacist 1/4). "We can't relax from checking" (pharmacist 2/4). "Patients expect to see us in 5-10 minutes. This is frustrating. They don't understand" (pharmacist 2/7). "I feel diluted as a professional, because dispensing requires 100% attention, leading to conflict at the degree of visibility we have" (pharmacist 1/3). "Pharmacists should be consulting and advising but have to check dispensing also. The role needs to be separated" (pharmacist 1/4). |
Box 1: Pressures in the workplace that impact on building caring relationships [30]
7.2.2 Patient-centred professionalism—managing external forces
According to pharmacy staff, Standard Operating Procedures (SOPs) in each pharmacy must be adhered to in all circumstances, in order to be accountable for one's actions: "[company name] always follow SOPs. If anything goes wrong they refer back. The system must be followed" (pharmacy staff 1/2). Pharmacists, particularly those working within larger stores, saw work as under corporate control, paid according to corporate financial structures, with jobs that evolved according to output-oriented measures. Within the larger companies, professionalism was synonymous with good management, and pharmacists and their staff expected to reprioritise tasks to achieve competitive retail figures, whilst complying with company policy. Patients are aware of the dual nature of the pharmacist's role and some of the pressures companies place upon pharmacists: "pharmacists are trying to balance retail and dispensing" (patient 1/4) as well as the impact that this can have on patient-centred services: "they have to compromise patient-centred professionalism to do both aspects of the job" (patient 1/4). However, this appears less at the forefront of the patient's mind than that of the professional's, and pharmacists link policy-drivers directly to problems of balance between healthcare and commerce. [31]
Stakeholders described the constant pressure on pharmacists to comply with company rules and achieve corporate targets: "pharmacists must think about business and the pharmacy in making money" (stakeholder 1/4). Moreover, pharmacy staff resisted companies dictating to practices in individual premises, noting that it was the pharmacy manager or support staff, not the company, who knew what was best for the local community. They suggested companies were making mistakes in their decisions about the use of space and working practices, giving as an example the large stock of sales items that normally ended up on the shelves: "Managers know their customers well. They should have more control. We were told to stock certain things then we end up selling them at half price, throwing good money away" (pharmacy staff 1/4), [32]
Pharmacists described the difficulties of balancing expectations of patients and companies. Whilst SOPs provided a framework for their work, being flexible enough to incorporate them and patient-centred professionalism at one and the same time was challenging. Some of the longer-standing pharmacists reflected that twenty-five years ago the Code of Ethics (DALE & APPELBE, 1989) had brought flexibility into the workplace. The pharmacists reflected that the current Code has introduced rigidity and underplayed their independent nature (ROYAL PHARMACEUTICAL SOCIETY OF GREAT BRITAIN, 2008). This was exacerbated by companies being too prescriptive: "Everything about my job is following the guidelines and rules. While that means I am able to do my job easily, I am not being creative or innovative, especially in dispensing" (pharmacist 1/1). [33]
Pharmacists were concerned that policies and guidelines were misleading and counter-productive, impinging on patient consultation. For example, pharmacists were expected to value the consultation but at the same time minimise interaction in order to maximise profit. Consequently, guidelines that used to be professionally driven were now enforced externally to little effect. This not only reduced pharmacists' professional freedom, it also diminished their autonomy and interest in the job. Within the context of ever growing legislation and concerns about litigation, pharmacists felt "anxious" (pharmacist 1/2) and "isolated" (pharmacist 1/3). [34]
7.2.3 Patient-centred professionalism—The effects of space and environment
Having considered the bio-photographic material, participants saw the influence of environment on patient-centred professionalism very differently. Pharmacy staff, for example, discussed their impressions of space in relation to both the people working in those spaces and the population groups they served: "rural or urban, rural need to keep more things in the shop for convenience" (pharmacy staff 1/4), and "it depends on the people coming through the door; in affluent areas the homely, less-clinical look may be better" (pharmacy staff 1/3). For the pharmacy staff, spatial arrangements and impressions of space were clearly linked to the populations being served. [35]
Patients, on the other hand, considered environment in relation to the different kinds of people who worked in different healthcare settings, not the different members of the public entering those settings, or urban-rural considerations. They were less concerned about the look of the premises and sceptical about whether pharmacists could ever display a fully patient-centred professionalism approach in their work, despite changing the pharmacy arrangement and function. Patients described the pharmacist as immersed in medication provision and medication development. Patients referred to the pharmacist's work as the "nuts and bolts, pills and potions, working with materials which years of research have produced" (patient 1/4). GPs, on the other hand, were involved in a job that was "person-oriented. They think about the physiology and what is wrong with the person. I wouldn't want to be a pharmacist. They do a job with no initiative" (patient 1/4). [36]
As with the pharmacy staff, stakeholders recognised that pharmacies and GP surgeries attracted very different kinds of people, and, to a degree, professionalism was based on who came through the door. However, unlike pharmacy staff and patients, stakeholders valued the spatial arrangement and function, contending that it was the environment that had the major impact on professionalism. In general practice, spatial arrangement developed through clearly delineated workspaces and clear professional hierarchies, and differentiated roles: "everyone knows what the GP does, they see them on TV in soaps; they save lives" (stakeholder 1/5). Community pharmacies, on the other hand, develop according to unclear boundaries and unclear roles: "what the pharmacist does is never seen" (stakeholder 1/5). This situation has been exacerbated by the new contract which has led, particularly in larger establishments, to open-plan spaces: "you can ask anything, see anyone" (stakeholder 1/3). Stakeholders and pharmacists described the breaking down of boundaries as unintentionally detracting from patient-centred professionalism, leading to public perceptions that all staff are interchangeable: "the customer picks the person who makes eye contact … They just want to speak to someone, not specifically the pharmacist" (stakeholder 1/4), And: "pharmacists observe patients and patients observe pharmacists" (pharmacist 1/6). Consequently, pharmacists were seen as less professional than their GP counterparts, with accessibility counterintuitively detracting from, rather than encouraging, patient-centred professionalism. [37]
Stakeholders also pointed to the emphasis on retail sales, in the pharmacy workspace, with a mixed-bag of display items on the counter and shop floor, unlike the GP surgery. Whilst pharmacists could do little more than present themselves as shopkeepers, GPs could present themselves as diagnosticians and consultants:
"[UK] Pharmacists don't help themselves in one way. They have bargain bins, it is not professional. The first image is of a shopkeeper, not a health professional. Pharmacies in [mainland] Europe are much better. They are dispensaries with health related products" (stakeholder 1/1).
"GPs are making money but it doesn't feel like it. Pharmacists think about business and the pharmacy making money and it shows. That is a huge perception difference" (Stakeholder 1/4). [38]
All groups talked at length about the look of the premises, particularly their shoddy, cluttered and claustrophobic appearance and in many instances, their old-fashioned ambiance. This was particularly evident in more rural areas, as well as some of the smaller, urban shops, where items were pilled high in every conceivable space. To some extent, patients accepted that it had to be like this because of the pharmacist's retail requirements. Patients justified this approach in relation to the two professions' very different roles:
"I am surprised that GP and pharmacist should be related. I see them as two distinct roles. I would not expect the same relationship with GPs and pharmacists … I want different things to take place and I am surprised that the professions should be regarded as equal" (patient 1/1). [39]
However, patients remarked on how cluttered space did not appear professional: "pharmacists have lots of 'goods' and you have a different impression of pharmacists, which lessens the importance of the pharmacist as a medical man" (patient 1/4).
|
"There is litter on the floor. That is not a professional image. You have to make the area look professional if you want to be treated professionally" (stakeholder 1/1). "Depressing, dark, dismal, too cluttered, can't see customers. I wouldn't like to work there" (pharmacy staff 1/1). "Horrendous, very claustrophobic, some of the conditions are so cramped. I wouldn't want to work in these conditions. My pharmacy is very open. We know our roles. Everything is efficient. I can't see that here" (pharmacy staff 1/2). "[The bio-photographic data were] surprising. A little depressing, frustrating, they sounded negative about their feelings, space and pressure, more so [with the] pharmacists than [with the] GPs" (patient 1/2). "The pharmacy is very cramped. All the medicines there [pointing to the photograph]. Pharmacists seem to be very self-important, seeing customers as an intrusion to work. They should have 1 person to sell and the pharmacist should be behind the counter" (patient 1/1). "Pharmacists want to make a profit. They pay out less on their environment (patient 1/3). GPs see patients as a whole, with all their ailments. Pharmacists are just delivering medication, based on the GP visit" (patient 1/5). "[Pharmacist] has a 'virtual' barrier. They have separated from the patient as they have to do their work. They have to compromise patient-centred professionalism to do both aspects of the job" (patient 1/6). |
Box 2: The look of the community pharmacy [40]
While stakeholders concentrated on the changing role of pharmacists in relation to changes in workspace arrangement, they also discussed the environment of the pharmacy and the need to acquire better people skills, through early career training. Pharmacy staff thought training was adequate and of a professional level, but stakeholders were sceptical that trainees, particularly pharmacists, had the basic social skills necessary to ever present a patient-centred professionalism approach. Rather, they saw trainees as having good qualifications and a firm grounding in science, but clinical orientation to the exclusion of all else. In addition, they described the professional "type" entering pharmacy as not the type to be comfortable with consultation. Pharmacists put lack of people skills down to the training programme itself, which they saw as: "woefully inadequate" (pharmacy 2/4). Pharmacists agreed with stakeholders that the curriculum was science-based rather than person-based, denying students the basic courses in helping others, like first aid, with breadth rather than depth of understanding. Whether training or character, this may go some way to explaining why, despite the new remit, consultation skills like consultation rooms are not being fully utilised.
|
"Pharmacists are not using the consulting rooms" (stakeholder 1/4). "You are taught communication and not consultation" (stakeholder 1/3). "Consulting rooms are put in wherever there is a space. No thought has been put into it. Patients may not want to go into the consulting room" (stakeholder 1/2). "We could use space differently if we had time to use the consulting space. You can't give your full concentration to both jobs" (pharmacist 1/4). "Some pharmacists are not good at communication or people skills. They have no eye contact and are miserable" (stakeholder 1/5). "The pharmacy degree [course] attracts 'nerds'. High qualifications are needed. It does not attract people with good communication skills" (stakeholder 1/4). "There's a conflict of interests. GPs have a very professional style of consultation. Pharmacists you can ask anything. They are trying to balance business with the professional side" (stakeholder 1/3). |
Box 3: Consulting in the community pharmacy [41]
7.2.4 Patient-centred professionalism—Different roles and expectations
Pharmacist as "shopkeepers" rather than as "patient-centred health professional" was the response participants gave to the bio-photographic data, in stark contrast to their impressions of GPs and their workspace. Pharmacists defended this position to an extent, by emphasising that GPs could design their own spaces, whilst concentrating on patient need through timely, well-organised appointments. Pharmacists were unable to relax from checking prescriptions or conducting MURs. They were pressurised by patients' unrealistic demands to consult at any time of the day, normally without having a fixed appointment:
"Time factors impact the time you can allow each patient. GPs have appointments. Their day is structured. Pharmacists have to see who walks through the door on any day. Pharmacists can't really plan … If we had more of a structured day we could focus more on the patient" (Pharmacist 2/1). [42]
As a result, pharmacists could not relax or explore the full extent of patient issues, leaving them frustrated and alienated, wanting to escape to the dispensary or consultation room when it was not in use for "time out", and rid themselves of more insistent clients. Though they recognised the importance of getting to know patients better, through both informal and formal consultation, the consultation room as a "refuge" for the pharmacist rather than as a "consultation space" for the patient was for many the preferred option.
|
"GPs have appointments. The[ir] day is structured" (pharmacist 2/1). "We are very restricted by the companies we work for" (pharmacist 1/3). "Doctors don't work for companies" (pharmacist 1/4). "Doctors have their own space and can organise it how they like. Pharmacists can organise to a degree, but are restricted by company rules and regulations. Some things are imposed. For example, I have to order things by their generic name. I am not always able to work in the way I want. As a pharmacist I couldn't have plants and personal items unless I have approval. What I can do is guided by the company" (pharmacist 1/2). "Patients can choose to go elsewhere to another pharmacist so we could lose the business. This is not so for GPs" (pharmacist 1/3). |
Box 4: Differences in GP and community pharmacy roles [43]
Patients emphasised differences between GPs and community pharmacists in terms of their different approaches to practice. GPs took medical histories and built up relationships with patients over time, taking the initiative with diagnosis and prescribing, and making recommendations for long-term care. Pharmacists were more restricted in all these aspects. In some cases they had no knowledge of the person entering the pharmacy, were limited in the time they could spend with clients and the extent to which they could prescribe medicine. In addition, whilst GPs were driven by what they prescribed, pharmacists were driven by the sales of what GPs prescribed; a subtle yet essential difference that affected their professional standing to the core. [44]
This in-depth, qualitative, consultation study has begun the process of clarifying "patient-centred professionalism" in modern-day, UK community pharmacy. This is in line with current interests in this subject worldwide (for example: HILL, 2000; DROEGE, 2003; WILLIAMS, 2007; PHARMACY PRACTICE RESEARCH TRUST, 2009), and in how pharmacy education can play a part in enhancing patient-centredness (BOYLE, BEARDSLEY, MORGAN & RODRIGUEZ DE BITTNER, 2006; PHARMACY PRACTICE RESEARCH TRUST, 2009). [45]
Our research investigated what the concept meant to professionals and the public and which elements of professionalism were particularly valued. Whilst our ongoing study will embellish these findings, we can already see not one but many definitions emerging through nuanced, complex, relational sets of ideas. These are dependent on personal positioning (professional or public), individual expectation, and different patient experiences of community pharmacy, as well as shared, group knowledge. Definitions change according to whose positions are being upheld at any given time, and which elements of practice, setting or interaction are being described: the pharmacist's day, the public's experience, the pharmacy environment, the direction the pharmacy profession is moving, etc. Thus the concept cannot be defined in any singular or stationary sense, but rather should be seen as a "moveable feast", best understood through the everyday examples of practice and interaction, in terms of whose experience is being expressed, and whose needs are being considered. The phrase is being mobilised by a whole series of interests and stakeholders to reshape practice, the effect of which remains both uncertain and contested. [46]
Patients clearly prioritise a quick and efficient dispensing service, provided by approachable and knowledgeable pharmacists expecting pharmacists to be available as and when necessary. Irrespective of pharmacy environment, if dispensing is timely and advice-giving appropriate, patients feel supported and well-served. Pharmacists are well-matched with this with respect to dispensing being the defining aspect of their work, and see effective dispensing as evidence of patient-centred professionalism. However, whilst taking particular pride in their technical skills, they are unhappy about patients' expectations of immediate accessibility. Indeed, pharmacists rail against an increasingly demanding public and overtly formalised consultation that takes them away from dispensing. Interestingly, this runs counter to the findings of EDMUNDS and CALNAN (2001), whose study (on reprofessionalisation of community pharmacy) indicated that pharmacists were keen to extend their roles into: "the domains that have traditionally been perceived as belonging to the medical domain" (p.949). EDMUNDS and CALNAN commented that despite a tendency to attribute ultimate authority to doctors, pharmacists wanted to become more patient-oriented. Our study has identified a reversal of views since 2001, and in light of the current emphasis on patient-centred values in pharmacy this may be of concern (ROYAL PHARMACEUTICAL SOCIETY OF GREAT BRITAIN, 2008). However, the turn-around may be better understood if we take into account workload pressures and pharmacists' inability to reconfigure the traditional role of dispensing whilst at the same time increase the patient-centredness of their role. For pharmacists, expectations that they be more patient-focused appear to compromise their sense of personal integrity and professional self-identity. [47]
Changes in patient expectation regarding the immediacy of service provision, alongside stringent company regulations have increased pharmacists' anxiety, leaving many of them overwhelmed and demoralised. They feel a loss of pride in professionalism and turn away from patients to escape to the dispensary or consultation room. They reflect nostalgically on the time before manifold, external demands, when they could function according to their vision of professionalism within the sanctuary of the dispensary, perfecting technical skills and ensuring an orderly medication through-put. With additional managerial tasks and company requirements to boost retail sales and change health-service delivery, this is a professional group with a diminished sense of self-respect. These findings are in line with Kevin Frank WILLIAMS' (2007, "professionalism in South African pharmacy"), who indicated that over-regulation of product pricing, and product-for-profit corporate approaches has negatively impacted on professionals' sense of autonomy. [48]
The professionals' descriptions of the disempowering effects of environment on practice indicate that neither open-plan space nor old-fashioned, cluttered, ramshackle space (the absent-minded shopkeeper) is entirely welcome. Here is a professional group clearly unhappy with both extremes of design, seeing them as preventing rather than enabling patient-centred professionalism. Moreover, the mixture of retail and dispensing highlights fundamental problems in the smooth running of the pharmacy. Whilst patients insist it is down to the people running the spaces rather than spaces themselves, pharmacists argue that they cannot provide the services patients require because they are victims, not leaders, of stylistic and process-driven change. Pharmacists and stakeholders see change as enforced by out-of-touch, output-orientated company managers, with unreasonable goals in the name of financial gain, leaving professionals torn between the familiarity of dispensing and informal advice-giving, and the unfamiliarity of formal advice-giving, within nondescript, corporate workspaces. They seek alternative professional roles to break free of the shackles of managerial responsibility. [49]
Djenane RAMALHO DE OLIVEIRA and Sarah SHOEMAKER (2006) presented a six-step approach to encouraging patient-centredness in pharmacy practice, including reflective listening, questioning, and recognition of behaviour and expectation. They argued that a current shift in focus from pharmacist to patient heralds an urgent need to change both the pharmacists' mindset and their practice. Whilst we agree that we should reconsider patient-centred professionalism within current practice, this study highlights the more urgent need to consider how change has led to a sense of despondency and disillusionment amongst professionals, and how to counter that. If there is such a number of divides between patient, corporate and professional need, how do we bridge that gap and bring about closer alignment? We would also suggest that whilst considering the different group positions in relation to this multi-facetted, complex notion, the stepped and regimented approach of Djenane RAMALHO DE OLIVEIRA and Sarah SHOEMAKER may be too linear to account for the nuanced disclosure of the concept this study revealed. Rather, we propose each facet could be considered in its fullness: environmental, relational, practical, spatial, personal, institutional, etcetera, and that in relation to each, the positive and challenging aspects of practice that have been aired are highlighted, so that professionals can know for themselves how workspace and practice could support or hinder their experience. Like Marcus DROEGE (2003) we recommend the introduction of the topic at an early career stage, and we agree that this should include personal reflection, problem-based learning and collaborative teamwork. We would recommend teaching that, in line with the more humanistic problem-based learning approaches (BARROWS & TAMBLYN, 1980), is supported by a set of schemas or templates with problem scenarios built in that we will identify through ongoing investigation, emphasising exemplars of best and challenging situated practices. This could be reinforced through CPD throughout the pharmacist's career to ensure enhanced people skills that are sustainable. Schemas should cover issues spanning the range of definitions of patient-centred practice that this study has begun to identify, matching them to the trainee or registered pharmacist's knowledge-base. [50]
We would like to thank the PHARMACY PRACTICE RESEARCH TRUST for funding this study. We would also like to thank workshop participants for giving their time to the study. We would like to acknowledge the administrative and organisational skills of Vicky DAVIES and thank her for her support of the project.
Appendix: Bio-photographic Material from UK Community Pharmacy
Example 1: Pharmacy A

Most of my time is spent within the dispensary. This is what I would consider the "nerve centre" of the pharmacy where all
the prescriptions are dispensed and where associated functions are carried out. The dispensary is a busy and pressured environment
and, in order to cope with the work load, I would usually work with three or four technicians. The physical dimensions of
the dispensary are not large, and therefore the number of staff in this relatively small area can create a feeling of claustrophobia!

The consultation room which we have sits just off the dispensary, so I am again able to access this whilst remaining relatively
close to the dispensing process. It is well placed to invite people into for a whole consultation, and also if I feel that
greater privacy is needed after a consultation has commenced in the quiet area of the shop. Because of the demands of the
dispensing workload, I try to keep the number of long consultations (longer than 15 minutes) to a minimum, without at the
same time making the patient feel that they have been rushed or that they have not been taken seriously. This is mainly done
through the use of body language within the particular space where the interaction is occurring at the time.
Example 2: Pharmacist B

This may seem a slightly depressing way to start this biography, but space within a pharmacy is, and will always probably
be, determined overall by one factor—money. Community pharmacies are businesses, and the goal of any business is make a large
a profit as possible. Community pharmacy mainly generates money from two different areas, counter sales and dispensing. Many
people still do not realise the potential valuable source of information that their pharmacist can be. Indeed, it is normally
down to the skill of individual pharmacists to build this reputation, which can take a considerable time. If the average person
on the street was asked "Who would be your first port of call for medication queries?", the answer would most likely be GP.
In a way, the lay out of the pharmacy can hinder the pharmacist' reputation as a healthcare professional, when the first thing
a person sees is the "special offer bin".
The design of an "open plan" dispensary (i.e. one where people can see their prescriptions actually being dispensed) is one
that has been more and more regularly adopted over the years and works well in my pharmacy. If people can actually see their
prescriptions being worked on and the staff running around as if they are on fire, then they will tend to be more tolerant
if the waiting time exceeds their expectations. It also makes the staff and pharmacist seem more accessible, which is what
is needed if the pharmacist is to promote their clinical skills.
1) In this paper the terms: public, customer, patient and client are used interchangeably. <back>
2) A number chosen to define a range whilst remaining manageable and understandable. <back>
Barrows, Howard S. & Tamblyn Robyn M. (1980). Problem-based learning: An approach to medical education. New York: Springer.
Blenkinsopp, Alison; Tann, Jennifer; Evans, Amanda & Grime, Janet (2008). Opportunity or threat? General practitioner perceptions of pharmacist prescribing. International Journal of Pharmacy Practice, 16(1), 29-34.
Blenkinsopp, Alison; Bond, Christine; Celino, Gianpiero; Inach, Jackie & Gray, Nicola (2007). National evaluation of the new pharmacy contract (Executive Summary). Pharmacy Practice Research Trust, http://www.rpsgb.org/worldofpharmacy/research/pharmacypracticeresearchtrust/ [Date of access: 03/21/2008].
Bloor, Mick; Frankland, Jane; Thomas, Michelle & Stewart, Kate (2001). Focus groups in social research. London: Sage.
Bohm, David (2004). On dialogue. London: Routledge Classics.
Boyle, Cynthia J.; Beardsley, Robert S.; Morgan, Jill A. & Rodriguez de Bittner, Magaly (2006). Professionalism: A determining factor in experiential learning. American Journal of Pharmaceutical Education, 71(2), 31.
Braun, Virginia & Clarke, Victoria (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77-101.
Chapple, Mary & Murphy, Roger (1996). The nominal group technique, extending the evaluation of students. Assessment and Evaluation in Higher Education, 21(2), 147-59.
Claxton, John D.; Richie, J.R. Brent & Zaichkowsky, Judy (1980). The nominal group technique: Its potential for consumer research. The Journal of Consumer Research, 7(3), 308-313.
Dale, Joseph R. & Appelbe, Gordon E. (1989). Code of ethics. In Joseph R. Dale & Gordon.E. Appelbe (Eds.), Pharmacy law and ethics (pp.217-218). London: Pharmaceutical Press.
Delbec, Andre L.; Van de Ven, Andrew H. & Gustafson, David H. (1975). Group techniques for program planning. Glenview, IL: Scott, Forsman, and Co.
Department of Health (2005). Implementing the new community pharmacy contractual framework information for PCTs. London: Department of Health.
Department of Health (2008). Pharmacy in England: Building on strengths delivering the future. London: Department of Health.
Droege, Marcus (2003). The role of reflective practice in pharmacy. Education for Health, 1(16), 68-74.
Edmunds, June & Calnan, Michael W. (2001) The reprofessionalisation of community pharmacy? An exploration of attitudes to extended roles for community pharmacists amongst pharmacists and General Practioners in the United Kingdom. Social Science & Medicine, 53(7), 943-955.
Epstein, Ronald M. & Hundert, Edward M. (2002). Defining and assessing professional competence. JAMA, 287(2), 226-235.
General Medical Council (2005). GMC Education Conference, http://www.gmc-uk.org/doctors/licensing/info/ebulletin/2005_05.asp [Date of access: 10/16/2009].
Gordon, Jill (2003). Fostering students' personal and professional development in medicine: A new framework for PPD. Medical Education, 37, 341-349.
Hill, Wendell T. (2000). White paper on pharmacy student professionalism. Journal of the American Pharmaceutical Association, 40(1), 96-102.
Kearns, Robin A. (1991). The place of health in the health of place: The case of the Hokianga special medical area. Social Science & Medicine, 33, 519-530.
Lloyd-Jones, Gaynor; Fowell, S. & Bligh, John G. (2002). The use of the nominal group technique as an evaluative tool in medical undergraduate education. Medical Education, 33(1), 8-13.
Miles, Mathew B. & Huberman, A. Michael (1994). Qualitative data analysis. London: Sage.
Pharmacy Practice Research Trust (2009). Call for proposals: Research into professionalism in pharmacy practice, 30 January 2009, London: PPRT, http://www.pprt.org.uk/Documents/TrustNews/Call_for_proposals_-Research_into_professionalism_in_pharmacy_practice.pdf [Date of access: 02/17/2009].
Picker Institute, Oxford (2008). Patient centred professionalism, http://www.pickereurope.org/ [Date of access: 01/25/2009].
Pike, Hannah (2007). Are consultation areas worth the investment? The Pharmaceutical Journal, 278, 24th February 2007, http://www.pharmj.com/Editorial/20070224/retailpharmacy/p1consultationareas.html [Date of access: 10/16/2009].
Pope, Cathy; Ziebland, Sue & Mays, Nick (2000). Qualitative research in healthcare: Analysing qualitative data. British Medical Journal, 320, 114-116.
Quinn Patton, Michael (1990). Qualitative evaluation and research methods (2nd edition). London: Sage.
Radley, Allan & Taylor, Dianne (2003). Remembering one's stay in hospital: A study in photography, recovery and forgetting. London: Sage.
Ramalho de Oliveira, Djenane & Shoemaker, Sarah J. (2006). Achieving patient centeredness in pharmacy practice. Journal of the American Pharmacists Association, 46(1), 56-66.
Rapport, Frances; Doel, Marcus A. & Elwyn, Glyn (2007). Snapshots and snippets: Reflecting on professional space. Health & Place, 13, 532-544.
Rapport Frances; Doel Marcus A. & Wainwright, Paul (2008a). "The doctor's tale": Enacted workspace and the general practitioner. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 9(2), Art. 2, http://nbn-resolving.de/urn:nbn:de:0114-fqs080227 [Date of access: 05/29/2008].
Rapport, Frances; Doel, Marcus A. & Jerzembek, Gabi S. (2008b). "Convenient space" or "a tight squeeze": Insider views on the community pharmacy. Health & Place, 15, 315-322, DOI: 10.1016/j.healthplace.2008.06.002.
Rapport, Frances; Doel, Marcus A.; Elwyn, Glyn & Greaves, David (2006). From manila to monitor: Biographies of general practitioner workspaces. Health: An Interdisciplinary Journal for the Social Study of Health, Illness and Medicine, 10(2), 233-251.
Robson, Colin (2002). Real world research. Oxford: Blackwell.
Rose, Gillian (2000). Practising photography: An archive, a study, some photographs and a researcher. Journal of Historical Geography, 26(4), 555-571.
Royal Pharmaceutical Society of Great Britain (2007a). Pharmacy 2020, http://www.rpsgb.org/worldofpharmacy/currentdevelopmentsinpharmacy/pharmacy2020 [Date of access: 02/01/2008].
Royal Pharmaceutical Society of Great Britain (2007b). The principles of pharmacy education and training, http://www.rpsgb.org/acareerinpharmacy/educationpolicy/ [Date of access: 03/07/2008].
Royal Pharmaceutical Society of Great Britain (2008). Code of ethics for pharmacists and pharmacy technicians. Medicine, Ethics and Practice, 32. London: RPSGB, http://www.rpsgb.org/pdfs/coeppt.pdf [Date of access: 08/22/2009].
Skoglund, Pär; Isacson, Dag & Kjellgren, Karin I. (2003). Analgesic medication—communication at pharmacies. Patient Education and Counseling, 51, 155-161.
Strauss, Anselm & Corbin, Juliet (1998). Basics of qualitative research: Techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage.
Welsh Assembly Government (2005). The community pharmacy contractual framework, NHS Wales Cymru, WAG, http://www.wales.nhs.uk/sites3/home [Date of access: 09/14/2008].
Williams, Kevin F. (2007). Re-examining "professionalism" in pharmacy: A South-African perspective. Social Science & Medicine, 64(6), 1285-1296.
Frances RAPPORT is Professor of Qualitative Health Research and Head of the Qualitative Research Unit at the School of Medicine, Swansea University, UK. She has written extensively about the scope of New Qualitative Methodologies for health research and is currently exploring the use of bio-photographic methods to clarify health professionals' reflections on inhabited workspace. Frances is also involved in a study using innovative narrative analyses with Holocaust survivor testimony. The study is exploring how notions of trauma suffering are presented in narrative form and what that tells us about survivor's ongoing healthcare needs.
Contact:
Professor Frances Rapport
Professor of Qualitative Health Research
Centre for Health Information, Research and Evaluation (CHIRAL)
School of Medicine
Swansea University
Grove Building, Singleton Park, Swansea SA2 8PP
Wales, UK
Tel.: +44[0] 17 9251 3497
Fax: +44[0] 17 9251 3430
E-mail: f.l.rapport@swansea.ac.uk
Marcus DOEL is Professor of Human Geography and the Head of the School of the Environment and Society at Swansea University. He is also an Associate Director of Swansea University's Centre for Urban Theory and a Fellow of the Royal Geographical Society and Institute of British Geographers. He has written extensively on social and spatial theory, and is the author of Poststructuralist Geography (1999, Edinburgh University Press), and the co-editor of Moving Pictures/Stopping Places (2009, Lexington) and The Consumer Reader (2004, Routledge). He serves on the Editorial Boards of Environment and Planning D: Society and Space and the International Journal of Baudrillard Studies.
Contact:
Professor Marcus Doel
Professor of Human Geography and Head of the School of the Environment and Society
School of the Environment and Society
Swansea University
Wallace Building, Singleton Park
Swansea, SA2 8PP
Wales, UK
Tel.: +44[0] 17 9220 3090
Fax: +44[0] 17 9251 3430
E-mail: m.a.doel@swansea.ac.uk
Hayley HUTCHINGS is a Senior Lecturer in Health Services Research at Swansea University. She has extensive experience of quantitative research methodologies related to health and has a special interest in respiratory conditions, patient health related quality of life, chronic conditions and the use of routine data.
Contact:
Dr Hayley Hutchings
Centre for Health Information, Research and Evaluation (CHIRAL)
School of Medicine
Swansea University
Grove Building, Singleton Park, Swansea SA2 8PP
Wales, UK
Tel.: +44[0] 17 9251 3412
Fax: +44[0] 17 9251 3430
E-mail: h.a.hutchings@swansea.ac.uk
Gabi JERZEMBEK is an ESRC-funded PhD student at the Cardiff Institute of Society, Health and Ethics (CISHE). She has experience in both qualitative and quantitative research methods and is interested in resilience and its link to well-being in the context of public health.
Contact:
Gabi Jerzembek
Cardiff Institute of Society Health and Ethics (CISHE)
Cardiff University
53 Park Place. Cardiff, CF10 3AT
Wales, UK
Tel.: +44[0] 29 2087 9161
E-mail: jerzembekg@cardiff.ac.uk
Dai JOHN is a senior lecturer in clinical pharmacy, law, ethics & practice at the Welsh School of Pharmacy, Cardiff University, UK. His major research focus explores and evaluates established, developing and novel roles of community pharmacists using qualitative and quantitative methodologies. Dai has, via several interdisciplinary collaborations, published widely on the public's use of medicines and advice from pharmacies.
Contact:
Dr Dai N. John
Senior Lecturer & Head of Clinical Pharmacy, Law, Ethics & Practice
Welsh School of Pharmacy
Cardiff University
Redwood, King Edward VII Avenue, Cardiff CF10 3NB
Wales, UK
Tel: +44[0] 29 2087 5804
Fax: +44[0] 29 2087 4535
E-mail: JohnDN@cardiff.ac.uk
Paul WAINWRIGHT qualified as a nurse in Southampton and had a range of jobs in the NHS before moving into Higher Education. He worked in the Centre for Philosophy and Health Care in Swansea University until 2005, which is where he developed his interest in the medical humanities. He is now Professor of Nursing in the Joint Faculty of Health and Social Care Sciences at Kingston University and St George's University of London. His research interests centre on the nature of practices in health care, from a philosophical and an empirical perspective.
Contact:
Professor Paul Wainwright
Associate Dean (Research) and Professor of Nursing
Faculty of Health and Social Care Sciences
Kingston University and St George's, University of London
Sir Frank Lampl Building, Kingston Hill Campus, Kingston upon Thames, KT27 7LB
England, UK
Tel: +44[0] 20 8547 8739
Fax: +44[0] 20 8547 8767
E-mail: pwainwright@gmail.com
Christine DOBBS completed her PhD at Swansea University in the area of social psychology in 2008. Her research interests embrace intergroup relations such as those between the health professional and service user, as well as relationships between different levels of staff in a professional setting. From the organisational psychology perspective, she is interested in the problems that may arise due to role conflict, and operative or organisational stress factors that may impact upon staff well-being.
Contact:
Dr Christine Dobbs
Research Officer
Centre for Innovative Ageing
School of Human Sciences
Swansea University
Singleton Park, Swansea, SA2 8PP
Wales, UK
Tel.: +44[0] 17 9260 2952
E-mail: c.dobbs@swansea.ac.uk
Stephen NEWBURY is an independent community pharmacist, having his own pharmacy in Mumbles, Swansea, where he is extensively involved in developing innovative patient-centred pharmaceutical care including healthy lifestyle support with health screening, allergy screening and care of the elderly. Having just qualified as an independent prescriber he is commencing an NHS commissioned service to support stable substance misuse clients; an area in which he has extensive experience.
Contact:
Mr Stephen Newbury
Community Pharmacist and Pharmacy Manager
The Pharmacy
Swansea
35-37 Newton Road, Mumbles, Swansea, SA3 4BD
Wales, UK
Tel.: +44[0] 17 9236 6120
E-mail: Stephen@intrapharm.com
Carol TROWER is the Professional Development Manager for The Co-operative Pharmacy, a multiple pharmacy chain of almost 800 community pharmacies across the U.K. A qualified pharmacist, with extensive experience in training and development of undergraduate pharmacy students, pre-registration trainee pharmacists, pharmacists and support staff, she has been involved in shaping the future of pharmacy training in the UK. With a keen interest in CPD and the revalidation of practitioners Carol has been part of the ROYAL PHARMACEUTICAL SOCIETY OF GREAT BRITAIN advisory group looking at revalidation of pharmacists in preparation for the introduction of revalidation in the near future.
Contact:
Carol Trowler
The Co-operative Pharmacy
Sandbrook Park, Sandbrook Way, Rochdale, OL11 1RY
England, UK
Tel.: +44[0] 78 3409 0810
E-mail: Carol.Trower@co-operative.coop
Rapport, Frances; Doel, Marcus A.; Hutchings, Hayley A.; Jerzembek, Gabi S.; John, Dai N.; Wainwright, Paul; Dobbs, Christine; Newbury, Stephen & Trower, Carol (2009). Through the Looking Glass: Public and Professional Perspectives on Patient-centred Professionalism in Modern-day Community Pharmacy [50 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 11(1), Art. 7, http://nbn-resolving.de/urn:nbn:de:0114-fqs100177.