

Volume 11, No. 1, Art. 22 – January 2010
Psychosocial Aspects of Speech Therapy with Head and Neck Cancer Patients: Clinical Experiences, Communicative Skills and the Need to Train Speech Therapists in Oncology
Peter Ullrich, Dorit Wollbrück, Helge Danker, Susanne Kuhnt,
Elmar Brähler & Susanne Singer
Abstract: Head and neck cancer patients suffer from high levels of psychological comorbidity and often do not receive adequate psychological assistance. Therefore, speech therapists are frequently confronted with specific psychosocial challenges beyond the scope of their standard professional education. The following aspects were examined via a mixed-methods approach to explore their own perceptions of these challenges and their skills to deal with them: 1) The experiences and problems of speech therapists working with head and neck cancer patients; 2) the self-assessment of speech therapists' skills in cancer patient care; 3) the experiences and observations of psychologists supervising case discussions in oncology with speech therapists; 4) the communication skills of speech therapists working with emotionally distressed patients in oncology
Our results show that therapists are acutely aware of their patients' distress. They agree that there is a need for patients to receive psychosocial counseling and that a significant portion of their speech therapy sessions is often dedicated to talking about personal problems. This difficult situation leads to: 1) deficiencies in speech therapists' ability to address patients' demands and deficiencies in distancing themselves from their patients; 2) speech therapists feeling overwhelmed with excessive demands and experiencing mental distress themselves.
The psycho-oncological knowledge and communication skills among speech therapists were often deficient in light of such demands. There is a need for further training in psychological and social skills for speech therapists working with head and neck cancer patients.
Key words: speech therapy; psychosocial oncology; head and neck cancer; training; psychic distress; communication
Table of Contents
1. Background and Problem
2. Methods
3. Results
3.1 Problematic areas for speech therapists working with oncology patients
3.2 Self-evaluation of strengths and weaknesses related to dealing with patients and their family members
3.3 Assessment by the supervisors
3.4 Communicative skills
4. Speech Therapy Between Demands and Excessive Demands—a Problem Matrix
5. Discussion and Conclusion
6. Problems and Limitations of the Study
Numerous studies have demonstrated that head and neck cancer patients are often in significant mental distress in addition to their physical problems (e.g. VAN'T SPIJKER, TRIJSBURG & DUIVENVOORDEN, 1997; MASSIE, 2004; ARCHER, HUTCHINSON & KORSZUN, 2008). Compared to other kinds of tumors, mental illnesses have often been determined within this group. In a study of tumor patients at a specialized hospital, 41.3% of head and neck cancer patients were diagnosed with mental illnesses (SINGER et al., 2007). In a study of 308 laryngeal cancer patients1) with tumor already diagnosed at a much earlier stage, the mental comorbidity was 19.8% (SINGER et al., 2008). [1]
The high level of emotional distress is not balanced by the use of a high level of professional psycho-oncology help at all. A study conducted on a group of laryngeal cancer patients revealed that only 1% was receiving psychological or psychiatric treatment. This means that there is an evident discrepancy between the various levels of distress and the actual use of care or help that is available, creating a strong under-supply of psycho-oncology and psychosocial care. [2]
In contrast, according to many experts, psychosocial care seems to often take place during speech therapy treatment sessions. The frequently intensive speech therapy usually starts immediately after primary treatment and often has the quality of psychosomatic primary care, even though speech therapists are not sufficiently qualified for this challenging task. In addition, speech therapists usually do not have regular supervision or peer-consulting groups to help them cope with the demands they are confronted with. [3]
The present study examines the unique work situation of speech therapists working in oncology. Here we focus on the therapists' perspective: the study aims to explore their perception(s) of such demands as well as their ways of coping with them. We combined various methods and perspectives to accomplish this. [4]
The following questions need to be answered in the context of this study (Section 3):
What experiences have speech therapists had working with head and neck cancer patients? What difficulties and problems do they see in this area of work?
How do they evaluate their own abilities to meet these demands?
What experiences and problems do supervisors of speech therapists working in oncology report?
What psychosocial, and communicative skills in particular, do speech therapists use? [5]
Our conclusions are devoted primarily to questioning whether and for which areas it is possible to deduce a need for continuing psychosocial education. [6]
In order to obtain the most comprehensive picture, various approaches—differing in methodical approaches as well as in sources—were combined. The main idea was to compare the evaluations made by the therapists and those made by others (experts, supervisors). [7]
The most important sources of data are 33 written interviews of speech therapists who worked with oncology patients. The sample consisted of registered individuals interested in a psychosocial continuing education program. The participants were recruited by using brochures distributed in head and neck cancer hospitals, rehabilitation clinics, oncology practices, conventions and in an article published in a scholarly journal (WOLLBRÜCK & DANKER, 2006). The participants were interviewed about their work with oncology patients and their competency when they signed up for the training (for demography, cf. Appendix 1). [8]
The questionnaires contained open questions designed to evaluate problematic areas in speech therapy work with head and neck cancer patients2) and the therapists' own evaluations of their abilities.3) 27 persons answered the questionnaires; their answers were then transcribed and coded using MAXQDA. In order to avoid theoretical over-determination of the material and to achieve the highest degree of openness possible in analyzing the problematic aspects of the profession under study, the coding was done inductively (MAYRING, 2000) and without theoretical categories about the study team by grouping similar materials and then creating thematic categories in an abstract and integrative way. This approach served above all to explore relevant subject areas (cf. ULLRICH, 2006). [9]
An outside perspective on the therapists' personal views on the problem was obtained through three problem-centered interviews with supervisors (psychological psychotherapists who combined their depth psychology orientation with an additional area of therapy emphasis—psychoanalysis, client centered psychotherapy, systemic therapy). The supervisors used a psychosocial course for speech therapists working in oncology ("PSYKOL," cf. WOLLBRÜCK & DANKER, 2006) to execute case oriented supervision of problems presented by the participants themselves. They divided the course participants into two small groups for a total of eight times, each time consisting in a two-hour session (a total of 32 supervisor hours), which they supervised. Summaries of the interviews were transcribed and coded as mentioned above according to qualitative content analysis. Due to the small number of expert opinions obtained in this way, the evaluation concentrated on the areas in which their assessments converged (ULLRICH, 2006). The interpretations presented here were provided to those interviewed for communicative validation (BORTZ & DÖRING, 2005, pp.328f.). This is based on the idea that these external experts should properly capture the speech therapists' evaluations; interpreting the subjective position of the supervisors was not the purpose of the analysis. [10]
The psychosocial competence was determined right before the beginning of the course through examination of discussion style preferences. The interviewees were asked to react to case vignettes in the questionnaire describing possible communication situations with emotionally distressed tumor patients in speech therapy. All contained a patient's statement to which an adequate answer should be presented. [11]
In order to obtain access to the various aspects of knowledge (active and passive), open and closed questions were combined.4) The interview subjects were invited to react to three case vignettes (situations with severely ill and emotionally distressed patients) in their own words (free answer test, N=27). The purpose of this activity was to analyze the active communication skills of the speech therapists. The written answers were transcribed and coded qualitatively and according to content analysis with the program MAXQDA. [12]
In addition, five further case vignettes with four answer possibilities on each were used in a multiple-choice setting. The instructions were simply to decide on an appropriate answer for each situation. With this approach it was possible to determine not situation-typical discussion behavior but a preference based on experience and/or knowledge of an answer style (KRAUSS, 2001, p.123). The distribution of discussion style preferences was determined using descriptive statistics (N=28).
|
Case vignettes (free answer test) |
|
67-year-old male, floor-of-mouth carcinoma, inpatient treatment due to healing difficulties: "Whenever my wife wants to visit me, I look forward to seeing her. But when she comes, we start quarreling." 51-year-old male, disadvantageous prognosis, before surgery: "What's gonna happen to my family, if I don't make it?" 66-year-old female, hypopharynx5) carcinoma, relapse: "I'm not going to be okay again, am I?" |
|
Case vignette (multiple choice test) |
|
53-year-old female, oropharyngeal6) carcinoma, has been in the hospital for two days: "I'm going to have surgery tomorrow. I am anxious." 69-year-old male, very bad general condition; therapy-resistant, metastatic floor-of-mouth carcinoma: "I'm getting worse. Seems like I'm gonna pass away soon." 68-year-old female, after surgery, often receiving visits of her daughters and grandchildren: "My roommate is always so cheerful, I cannot understand that!" 54-year-old male, sensitive, who received a good prognosis after a laryngeal resection: "You know, I'm a real failure! I hate myself because I do everything wrong!" 63-year-old male in relatively good general health, saying about the diagnosis at the head and neck cancer ward: "Do I have cancer?" |
Table 1: Case vignettes to evaluate communicative skills [13]
Inductive and deductive qualitative content analysis were combined when analyzing the answers to the free answer test in order to establish a set of categories of typical communication forms with head and neck cancer patients (MAYRING, 2000). The category system presented below is based on studies of KRAUSS (2001, p.XVII). It was developed there to assess communication style preferences of care staff when dealing with dying patients. These categories were developed to analyze situations involving emotional distress, and were therefore adequate for our study. The peculiarities of the study group and their areas of activity, however, demanded adjustment and expansion of the category system. Accordingly, the entire qualitative text material was analyzed in an open procedure of inductive category development (MAYRING, 2000). The existing category system was complemented with these results, and other categories without clear delineation were grouped together. Then, the category system was developed with the input of the participating researchers and a communications expert. All answers from the course participants were then coded again by two participating researchers. [14]
Inter-coder reliability was measured using ratio of coder agreement, which gives the percentage agreement of both coders.7) The entire inter-encoder reliability coefficient was R=.71. When there were disagreements over coding, the research group conducted a group coding session, in some cases using a communications trainer (consensual validation, cf. BORTZ & DÖRING, 2005, p.328). [15]
From these results, ways of dealing with difficult situations and emotionally distressed patients could be deduced. The results of various assessment steps were summarized in a matrix that substantiates specific continuing education needs (see Figure 2). [16]
3.1 Problematic areas for speech therapists working with oncology patients
The most obvious result is that every therapist who was interviewed clearly mentioned the high psychosocial demands related to working with tumor patients. Almost all interviewees agreed that head and neck cancer patients are often in emotional and social distress. They also agreed on the significant need for communication in the patient group, and on the fact that the work of speech therapists involves considerable discussion and counseling:
"The patient is very fixed on the speech therapist and talks about his worries and fears." (ID 038))
"Since every tumor has different consequences, each therapy constitutes a new and specific challenge not only from a professional but also from a psychosocial perspective. I, as a therapist, have a 30- to 45-minute session with a patient. They often have very high expectations and usually need the first hours to simply talk to someone." (ID 08) [17]
This situation, however, causes a difficult challenge for therapists, namely that of balancing the elements of speech therapy as their actual core task against psychosocial counseling and care:
"Creating boundaries between psychosocial/psycho-therapeutic care and therapy is likely to be the most common challenge." (ID 19)
|
Most important problematic areas |
|
High psychosocial distress of patients (decreased quality of life, anxiety, despair, depression, searching for meaning, guilt, problems related to body image, dependency, experiencing violence, difficult family situations, financial situation, social withdrawal, loneliness) High need for communication Finding a balance between speech therapy and psychosocial demands Role of family members and the difficulties related to bringing them into the therapy Personal boundaries and psychological hygiene Dissatisfaction with patient behavior Communication problems |
Table 2: Problematic areas for speech therapists working with oncology patients, seen from the perspective of the speech therapists [18]
The experiencing of these aspects as difficulties is also connected with subjectively experienced deficits in one's own professional abilities. Thus, the problems in therapist-patient communication and counseling were addressed openly by some interviewees. Some also reflected on the extreme emotional distress this creates for therapists and on the stress it creates for their own psychological hygiene as well as its impact on boundaries:
"The patients had phases of depression again and again (e.g. due to loss of taste) or because progress only seemed to occur gradually. In such a situation one needs inner strength and a positive attitude and view of life." (ID 04)
"Blows of fate of individual patients, e.g. when a tumor had not been found for months despite the visits of numerous physicians, sometimes strongly affect me as a therapist and make me very angry." (ID 26) [19]
No institutional resources such as supervisors or peer counseling are available to help therapists deal with such emotions. [20]
Further problematic areas were rarely addressed: difficulties in working together with other professionals (e.g. physicians), insufficient explanations provided to patients, feeling of excessive demands in one's own field (lack of specialized medical knowledge and knowledge of speech therapy) and time as well as financial restrictions for a successful therapy. [21]
Several interviews reveal a clear paternalistic perspective towards patients, whom the therapists criticize for their (from the therapists' perspective) inadequate actions and reactions. This produces negative feelings toward patients in therapists ("they make me very angry") when they see patients showing unsatisfactory loyalty to therapy as well as motivation ("lacking willingness to cooperate," "does not want to do anything about it," "inadequate conduct," "inability to change cancer-producing lifestyles"). Importantly, three interviewees had little or no problems working with emotionally distressed tumor patients, although they had registered for the course.9) [22]
3.2 Self-evaluation of strengths and weaknesses related to dealing with patients and their family members
The answers to the question about one's own strengths and weaknesses were divided into two areas: personality characteristics and professional aspects (conduct, work methods). The answers are rather heterogeneous, but presented quantitative overlaps. Table 3 presents an overview of the categories. Since most answers only had key words, similar concepts were summarized without us being able to ascertain the specific subjective content of the concepts.
|
|
Strengths |
Weaknesses |
|
Personality aspects |
Openness Empathy Further: initiative, ability to motivate, Respect for others, flexibility, psychological hygiene, honesty, realistic attitude or expectations |
Antipathy/prejudice toward certain patients One's own emotional state Further: too little money, fear of honesty, perfectionism, empathy |
|
Professional aspects |
Communicative skills General professional competency Further: boundaries, bringing in social surroundings, taking time, experience, therapy design, goal oriented, delivery of information to the patient, psychological and psychotherapeutical knowledge |
Boundary setting Further: timing, communication, reaching goals, psychological therapeutical knowledge, ethical questions, medical knowledge, general professional knowledge |
Table 3: Self-evaluation of strengths and weaknesses related to dealing with patients and their family members (in bold letters = frequent answers) [23]
When it comes to improving the situation of emotionally distressed oncology patients and therapists, weaknesses—whether therapists are aware of them or not—are most interesting. The most commonly mentioned weaknesses are generally those involving the therapists' personal states of mind or feelings. This has to do with boundary problems, which become apparent in prejudices or negative reactions to certain patients as well as with difficulties in one's general mental state. [24]
Personal evaluation of communication skills differs markedly from evaluations from an outside perspective. About half (13) of the interviewees consider their communicative skills as personal strengths. Yet, the communicative styles chosen by the group are not predominantly conducive. Only two of the interviewees' answers in the free answer section could be considered genuinely positive (compare section 3.4.2). For all others there were dominant to primarily non-conducive communication aspects that also had negative (weakening to neutralizing) effects on the conducive communication aspects employed. The same is valid for the self-assessment as "empathetic" and "open." These self-attributed skills were usually not confirmed in the free answer test. [25]
3.3 Assessment by the supervisors
Many aspects of the self-assessments and problematic areas coincide with the impressions gained by the supervisors working in casuistics with the speech therapists. These impressions are overwhelmingly consistent, although the external supervisors did not discuss the contents of the meetings with each other, and the individual supervisors also guided different course participants. They reported three main problematic areas characterizing the work speech therapists perform with tumor patients that sometimes make it more difficult: role conflicts, difficult subjects and closeness-distance conflicts. [26]
The first issue lies in the definition of roles. It was often difficult for the therapists to define and limit their work to the main task and content of the speech therapies. The high psychosocial demands led to conflicting roles between their relatively narrow main role as speech therapists and the expectations brought to them as counselors and persons of trust and confidence. Case histories often dealt with the following question (in the words of a supervisor): "Where does their job begin and where does it end?" There was also a need for clarification concerning one's own role within the health care system. [27]
The unusual challenges some patients bring along often carry a background for such role conflicts. Speech therapists showed a high need for relief and for exchanging thoughts on particularly difficult subjects such as severe illness, death and dying, feeling powerless, ill children, trauma and revulsion (through physical proximity, bad breath, bodily secretions, dilapidation), in order not to have to cope with these subjects alone. [28]
For such subjects, the closeness-distance conflict becomes even more urgent. All supervisors stated that the participants were generally highly committed and had a high professional and personal motivation, which often reverted into over-commitment. This was demonstrated in, for example, blurred professional boundaries, making offers for different kinds of relationships as well as agreeing to some sort of friendship relationship with patients, giving one's private telephone number, or assuring that the therapist was on call around the clock and, finally, the frequently occurring counter-transference of having strong sympathy with patients. The psycho-dynamic backgrounds of this problem ("helper syndrome") could not be easily brought into the therapists' self-reflection. [29]
Case history supervision could help bring a practical solution to some acute problems and create relief in speech therapists by fostering communicative exchange and pointing out as well as probing solutions for comparable future situations. The supervisors agreed on the speech therapists' high need for supervision and peer counseling. This need could be deducted through analyzing the problematic areas mentioned above, the great interest of the participants in discussion, exchange, networking and case history work as well as from their frequent wish to continue the case history sessions. This also results from their frequent professional loneliness: a large portion of the therapists participating in our study are said to be "lone warriors" and do not have professional supervision and—in the case of private practices—often do not have regular discussions about their work and the burdens associated with it. [30]
The supervisors agreed with this summary of their assessment of the supervisions as produced by the research team. [31]
3.4.1 The category system
Psychosocial demands become apparent during conversations between speech therapists and patients. How exactly does communication occur in difficult situations? First of all, we want to present our first conceptual result––the category system (cf. Appendix 2)––which gives an overview of the discussion styles used in difficult emotional situations. [32]
The coded communication styles were divided into three main areas, based on a normative distinction. For successful conversations in emotional situations, distinctions were made at the highest level of abstraction between conducive, non-conducive and other communication styles. This classification comes from a rich area of literature on communication between therapists and patients in oncology (cf. KAPPAUF, 2004 for an overview). However, studies and conceptual considerations have so far primarily examined the effects of the communications styles of physicians and care staff. As there exist no studies on speech therapists, we had to fall back on the aforementioned. [33]
The criteria for "conducive" were borrowed from the foundations of patient-centered communication. This is indicated in emotional communication situations in particular, since it primarily opens the floor for unpacking each individual's concerns. Other situations also demand using therapist-centered communication forms (LANGEWITZ, 2002), which require a structured approach based on criteria/knowledge systems that patients are not familiar with, as in differential diagnosis. The evaluation based on this categorization addressed concrete situational action contexts and was not a general normative classification of a speech action. [34]
3.4.1.1 Conducive communication styles
The communication styles given most attention and importance in literature are "empathy" and "further inquiry." They primarily function as ways to offer relief to patients by mirroring their emotions, understanding, containment, taking up their own language/metaphors and by exploring their feelings and needs (FOGARTY, CURBOW, WINGARD, MCDONNELL & SOMERFIELD, 1999). They also give patients the feeling that they "have been heard and understood" (KAPPAUF, 2004, p.1253, cf. also STIEFEL & RAZAVI, 2006, p.40). These styles aim to keep the floor open for communication to convey concerns and views of patients and take their subjective reality seriously (LANGEWITZ, 2002). Two other conducive communication styles serve to stimulate the patients' potential for understanding and improving their situation ("acceptance as self-expert") as well as the resources, abilities and plans of the patient ("resource- and future-orientation"). This is done without suggesting, influencing or becoming authoritative, which would amount to forcing therapists' interests upon patients (ULLRICH, 2010 in press, Chapter 5). [35]
3.4.1.2 Non-conducive communication styles
Among the communication styles considered disadvantageous, ethically problematic or non-conducive to feelings or to deal with distress, we find, in particular, those that do not take into account the specific individuality and the subjective situation-framing of patients, which hinders the understanding of patients' needs ("expert-interpretation," "generalization," "projection/identification"; see KAPPAUF, 2004, p.1255). This also occurs when the emotional content of communication is ignored ("defense," "rationalization") or when the personal integrity and the "right to understandable information" (KAPPAUF, 2004, p.1252) as the basis for an informed decision are violated ("command," "moralizing," "deficit orientation"). [36]
3.4.1.3 Other communication styles
The "other" categories contain statements that can be adequate or inadequate, depending on the context; they cannot be clearly evaluated with the selected instruments. In addition, this category also comprises various general aspects of communication that do not fit into normative standard distinctions but are nevertheless relevant to evaluate psychosocial continuing education needs for speech therapists working in oncology. [37]
The category "transferal to others" comprises all statements addressing the possibility of bringing in other staff/persons. Such communication, on the one hand, is an important moment in recognizing one's own professional and emotional limits, but, on the other, should not be used to avoid emotional situations simply by resorting to referrals to psychotherapeutic assistance options. The same is valid for "being speechless/helpless." This is a category capturing statements that mirror genuine excessive demands from patients (important for boundary setting) and replies to patient questions which cannot be answered (because of a lack of knowledge or competency). However, this should—from the perspective of patient-centered communication—not be used to simply avoid the concerns of patients or to externalize emotional components. The category "offer help" encompasses all personal help offers. The design of these offers and particularly the fact that they are limited to specific appropriate professional frameworks is important for the sanity of the speech therapist (boundary setting) and for the protection of the patient, when problems cannot be dealt with properly by speech therapists using the professional, emotional, or time resources available to them. [38]
3.4.2 Active communication skills
When testing the active communication skills, it became clear that both conducive and non-conducive communication styles play important roles in the communication repertoires of those interviewed. Yet, almost all interviewees often used non-conducive communication styles. Only 4 of the 27 interviewees opted exclusively or almost exclusively for conducive communication styles. Table 4 shows the frequency of individual communication styles.
|
Non-conducive |
Conducive |
Other |
|||
|
Expert interpretation |
19 (30) |
Further inquiry |
16 (25) |
transferal to others |
9 (12) |
|
Command |
11 (18) |
Empathy |
13 (21) |
Being speechless or helpless |
7 (7) |
|
Defense |
10 (13) |
Resource and future orientation |
2 (2) |
Offer help |
6 (8) |
|
Rationalization |
10 (14) |
Acceptance as self-expert |
1 (3) |
Encouraging |
4 (4) |
|
Generalization |
8 (8) |
|
|
|
|
|
Moralizing |
3 (3) |
|
|
|
|
|
Deficit orientation |
3 (3) |
|
|
|
|
|
Projection/ |
2 (2) |
|
|
|
|
Table 4: Distribution of communication styles (number of persons using a certain communication style, in parentheses the total frequency of each code, N = 27) [39]
Conducive communication styles
The communication styles "questioning" and "empathy" belonged to the conducive communication repertoires of about half of the therapists interviewed. The conducive communicative orientation toward the exclusive knowledge of the patients concerning their own lives and resources or future potential, however, hardly played a role. [40]
The following excerpt documents a 46-year-old therapist giving several answer possibilities—all conducive—to a vignette:
(66-year-old female, hypopharynx carcinoma, relapse): "I'm not going to be okay again, am I?"
"I can really understand that the bad news makes you sad.
Or: What do you think your chances to heal are?
Or: What can you do to increase your chances to heal?" (ID 19) [41]
The first potential answer signals understanding and empathy. The other two answers acknowledge the patient as a self-expert, thereby signaling options to act and self-efficacy to the patient, since the statement encourages her to give her opinions and assessments. In addition, a positive resource-oriented perspective was facilitated (instead of false suggestions) since the perspective on the question is guided toward potential developments. In addition, the question form that was chosen makes further statements from the patient possible. Nevertheless, such a relatively wide conducive communication repertoire presents an exception in the therapist groups under study. [42]
Non-conducive communication styles
"Expert interpretation" was the quantitatively most important among the negative communication styles (occurring with almost three-fourths of the interviewees). Other frequent styles were "command," "defense," "rationalization," and "generalization" (one-third of the interviewees for each). [43]
Sometimes, the interviewees only produced problematic reactions. The following may serve as an example:
(67-year-old male, floor-of-mouth carcinoma, inpatient treatment due to healing difficulties): "Whenever my wife wants to visit me, I look forward to seeing her. But when she comes, we start quarreling."
"Try to simply show your wife how much her visit makes you happy, and try to talk about the time after the hospital; maybe you could plan a trip together.
Ask your wife how she is coping with your illness, and make efforts so that you will also understand her.
At the moment the situation is difficult for both; in spite of this you should radiate confidence. Talk about the family a lot." (ID 12) [44]
Three negative categories were coded (command, rationalization, expert interpretation). First, the whole answer is very directing instead of encouraging the patient to express or develop their own perspectives; many clear suggestions are made that all come from the therapist's perspective and are not motivated by the patients' statements. The rationalizing orientation towards "practical solutions" negates the emotional content of the patient's statements and denies helpful empathetic recognition of dissatisfaction. In addition, the statements concerning the emotional condition of the partner are purely speculative. Also, the considerable amount of information overwhelms the patient. [45]
Positive and negative communication styles often overlap. In many cases the existing conducive aspects are canceled out or at least relativized through the non-conducive ones, as demonstrated by the following example:
(51-year-old male, disadvantageous prognosis, before surgery): "What's gonna happen to my family, if I don't make it?"
"Is this your first surgery? Are you afraid of not waking up from the anesthesia or that the illness is so bad that it cannot be taken out?" (ID 15) [46]
Here, the therapist appears to be interested in the patient's viewpoint. He/she shows interest and readiness to continue listening. The patient was given room to talk about the surgery and his/her possible fears. But the therapist gave no active effort to keep the floor open to discuss the patient's subjective viewpoint; he/she succumbed to the temptation to take possession of the space reserved for the patient too early. Two alternative answers were suggested that seem to address the emotional condition of the patient, but they were unnecessarily restrictive and were probably understood as arbitrary and as taking precedence over the patient. The communication offer was taken back, and the communication space closed. [47]
Other communication styles
In seven cases "speech-/ helplessness" was signaled. The ambivalence of this category (see above) becomes clear in quotes such as the following:
(66-year old female, hypopharynx carcinoma, relapse): "I'm not going to be okay again, am I?"
"I can't give you an exact prognosis; the doctor is responsible for that." (ID 02) [48]
The answer is factually correct. It is not the responsibility of the speech therapist to give a diagnosis concerning the course of the illness. Referring to the doctor's responsibility ended the discussion. This was meaningful to create one's own boundary to mark concerns that cannot be solved. The possible emotional aspects of the message (possible fear of death, worry, uncertainty, feeling not adequately informed or similar) did not receive any space in this quick rebuff. [49]
The same is true for the category "transferal to others" (a reaction to the same case vignette):
"… here there is the chance to get advice from a psychologist. He can talk to you about your worries and fears." (ID 04) [50]
This statement would be problematic only if the answers were given without empathy or further inquiry (which was not the case in this situation). [51]
The kinds of offers for help present in the answers are interesting. They ranged from straightforward organizational support as is frequently found in a hospital situation ("Should I make an appointment for you with the psychologist?") to very extensive offers that make it clear how difficult it is to set one's own boundaries. Both aspects are exemplified in the following excerpt:
(67-year old male, floor-of-mouth carcinoma, inpatient treatment due to difficulty healing): "Whenever my wife wants to visit me, I look forward to seeing her. But when she does come, we start quarreling."
"It is surely very difficult for each of you; if you want, I will gladly meet with both of you." (ID 10) [52]
This situation reveals a risk of trespassing professional boundaries. To protect the patient and the speech therapist (who is often not adequately qualified for such services and also not paid for them), persons with psychotherapeutic competence could be called upon. These problems present no single occurrence, as confirmed by the evaluations of the supervisors, the open answers to the case vignettes and the self-evaluations on the subject boundary setting and psycho-hygiene. The examples make it clear how difficult it is to bring ideals of the best possible care and help for patients in harmony with one's own psycho-hygiene and role security. [53]
3.4.3 Passive communication skills
All 20 possible answers (five vignettes with four answers each) of the multiple-choice tests were attached to a particular discussion style. Figure 1 shows a total of seven styles, of which five are non-conducive to communication and two (empathy, further inquiry) are conducive. We have depicted the total percentage of possibilities actually used to choose a particular style (see Figure 1).11) [54]
The study participants only seldom chose the non-conducive discussion styles (from 0 to maximally 18% in the different styles). In none of the presented case vignettes did they choose a defensive answer. In contrast, conducive communication styles were used more often. Of the possibilities to react with empathy or questioning, therapists actually made use of these possibilities in more than half of the cases. A conducive communication style was chosen in a total of 68% of the cases.
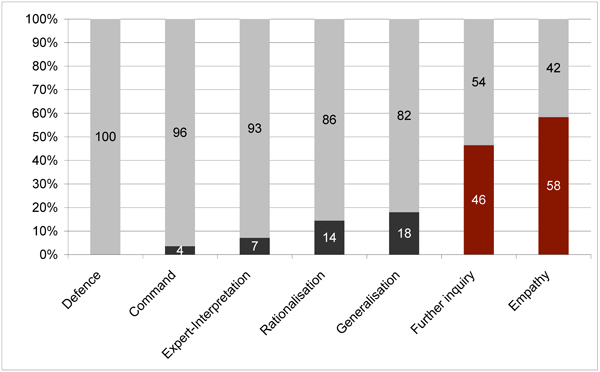
Figure 1: Discussion style preferences in the multiple choice test (N=28) [55]
4. Speech Therapy Between Demands and Excessive Demands—a Problem Matrix
The results presented here can be brought into a matrix that categorizes the most important difficulties in working with emotionally distressed tumor patients. This matrix was made possible by compiling the experiences and views of speech therapists, their supervisors', and the evaluation of their communicative skills.
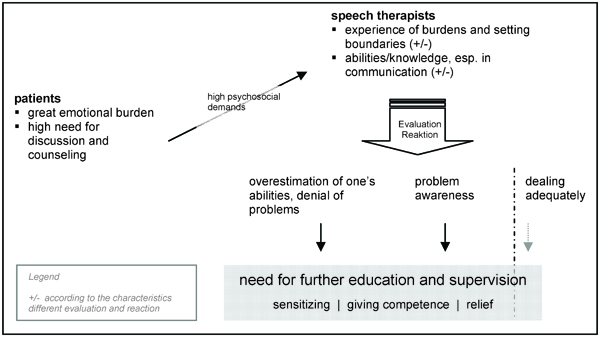
Figure 2: Speech therapy with distressed tumor patients between demands and excessive demands—problem matrix and need for
continuing education [56]
The high emotional distress of many head and neck cancer patients corresponds to a relatively low level of psychotherapeutic care. This often causes speech therapists to become important contact persons for their patients in psychosocial matters, which takes a lot of time in the speech therapy. There is a broad consensus on this. On the one hand, this affects the speech therapy aspects of the treatment. On the other hand, it presents a great challenge. The patients' emotional distress affects the therapists, who do not have adequate professional structures for their own psycho-hygiene (e.g. supervision, peer counseling). They end up bringing this distress home and experiencing it as emotional pressure. Finding relief is left to the individual. In addition, we have seen that counseling or additional psychotherapeutic competencies do not suffice to address the special challenges related to situations involving emotional distress. [57]
Three styles of dealing with this challenge have been observed. The first was labeled adequate handling of psychosocial aspects. This type is characterized by competent patient-centered communication in emotional situations, consciously taking care of oneself and setting boundaries as well as being aware of the potential and limits of one's own capabilities of psychosocial intervention. Disseminating this type of approach is constrained by personal and institutional limitations as reflected by the lack of continuing education and supervisory options as well as in funding and time restrictions in speech therapy. [58]
The second type can be labeled as problem aware. It is characterized by a subjective awareness of problems concerning distress (boundary problems, sensing pressure, prejudices, rage) and/or dissatisfaction with one's own professional knowledge and ability, which can be also be expressed in an explicit desire for continuing education. [59]
A number of those interviewed place high demands on themselves, which go as far as obvious overestimation of their own professional and personal-emotional possibilities (self-overestimating type). This becomes clear, on the one hand, in their communicative behavior, primarily in their preference for "expert-interpretation" and "command," where they overextend their competencies and, on the other hand, in their problematic personal boundary setting and lacking recognition of their own professional and personal/emotional boundaries, which is seen primarily in their offering help that often goes too far. This can go as far as completely denying the special challenges of working with the patient group under study. This type was represented, in its purest form, by only two of the interviewees. They stated that they saw no problems in this field of work but also tended to communicate using the non-conducive styles "command" and "expert-interpretation." [60]
Both aspects (present and absent awareness of problems) make the need for continuing education, which goes into various directions, clear. One direction addresses the problematization and sensitization to the special situation of taking care of emotionally distressed oncology patients and the difficulties attached to it. The other aspect encompasses conveying concrete knowledge and techniques in dealing with this situation. Supervision, peer counseling or other forms of actively dealing with the problems mentioned are generally needed independently of one's personal qualifications. [61]
The focus of this study was to explore the unique qualities of the work situation of speech therapists in oncology, since they often work without sufficient qualification to address the psychosomatic basic care needs of head and neck cancer patients. The results presented here support the thesis that work with emotionally distressed tumor patients presents a great challenge for speech therapists that they cannot optimally master without psychosocial support for themselves or continuing education. [62]
The central challenge for speech therapists is found in the continual balancing act of providing speech therapy in a narrow sense and addressing the considerable need for communication in patients. Conflicts emerge from this concerning the therapists' abilities and role definitions. Additionally, difficulties appear in keeping the professional distance-nearness relationship when dealing with emotionally distressed patients. Among some speech therapists in the study, there was also a discrepancy between their own assessment and the assessment of others concerning their strengths and weaknesses in dealing with patients. Yet, therapists can call on the rich experience, knowledge, and skills they already have. Weaknesses are juxtaposed to strengths, non-conducive communication styles to conducive styles. [63]
Other professional groups in the medical field (physicians, nurses) also show a lack of psychosocial knowledge and deficits in communication with oncology patients (FALLOWFIELD et al., 2002; MAGUIRE, 1999; PARLE, MAGUIRE & HEAVEN, 1997; RAZAVI & DELVAUX, 1997). These deficits are usually credited to a lack of continuing education, which also seems to be the cause here. [64]
A comparison with studies of the communication behavior of physicians suggests that improved communication between speech therapists and their patients would lead to greater satisfaction with treatment (FALLOWFIELD, 1995; MAGUIRE & PITCEATHLY, 2002) and to an improved emotional state for patients (FOGARTY et al., 1999; ROTER et al., 1995). Improved communication skills can also contribute to lowering distress as well as to a greater satisfaction with work for therapists (MAGUIRE & PITCEATHLY, 2002). The exact effects in speech therapists are still under study. [65]
From these results we can make initial suggestions regarding the general content of possible continuing education efforts:
Sensitizing for the emotional distress of patients and for the special challenges speech therapy faces in connection with patient distress.
Sensitizing for special emotional demands of therapists and, coming from these demands, the needs for setting boundaries and psycho-hygiene as well as concrete techniques for establishing these, and especially to prevent burnout.
Conveying knowledge and abilities to conducively and securely conceptualize the special psychosocial aspects of these therapies (recognition of emotions, reliable use of appropriate intervention and communication techniques, and expansion of repertoire of communication techniques to encourage conducive styles). [66]
It is the difference between a high level of passive knowledge and a lower level of active communication skills in the group under study that makes clear that such a continuing education program cannot be based simply on adversarial conveying of information. It has to contain practical exercises that would help teach the use of individual methods and techniques, which follows on other experiences in training programs in oncology (JENKINS & FALLOWFIELD, 2002). The current desire for continuing education is a good motivational basis for putting these ideas into practice. [67]
6. Problems and Limitations of the Study
The evaluations of the supervisors must be interpreted carefully, since the speech therapists worked together with them during continuing education; this means the supervisors' impressions of the therapists can also be based on the results of the supervisors' own interventions. [68]
In addition, it is also difficult to estimate which influences have resulted from the special composition of the sample. Since registration for the psychosocial course, which was required for admission into the study, can indicate a special need for continuing education and an existing sensitization to problematic areas in the course (which in a way cancels itself), and since the interviewees were found to be very heterogeneous in several aspects, we assume that we do not have a distorted picture here. [69]
One can also criticize a certain "artificiality" of the case vignettes and their written answers, which despite following a basically qualitative approach signal a certain affinity to experimental research designs. Yet this approach makes changes in the communicative competences in the course of time easier to verify and makes it possible to clearly evaluate the interventions—within the limits of this method. [70]
Further studies in and beyond oncology, especially probing and evaluating psychosocial training, are needed. Knowledge about the problem fields addressed here could be refined through representative statistical analyses (requiring larger numbers of participants) in similar designs or through a deeper qualitative examination in more natural communication situations. [71]
This study was made possible by a grant from the German Cancer Aid e. V.
|
|
|
N |
Mean value (Range) |
|
Professional experience |
25 |
9 years (1-25) |
|
|
Professional experience with head and neck cancer patients |
28 |
8 years (0-29) |
|
|
|
|
|
Mean value (Range) |
|
Age |
|
28 |
43 years (24-55) |
|
|
|
N |
Percent |
|
Gender |
female |
25 |
89 |
|
|
male |
3 |
11 |
|
Current professional situation |
Employed in practice |
1 |
4 |
|
|
Employed in hospital |
9 |
32 |
|
|
Independent in own practice |
14 |
50 |
|
|
Free lance in practice |
4 |
14 |
|
Previous experience with seminars of this type |
yes |
8 |
29 |
|
|
no |
20 |
71 |
Table 5: Demography of the interviewed speech therapists
|
Communicative style & definition |
Examples |
|
CONDUCIVE |
|
|
Empathy: reflect needs and emotions, use patient's language and metaphors |
You're worried about the development of your illness? |
|
Further inquiry: encourage patient to voice or specify wishes, needs, current condition, aims |
Have you mentioned that to your family? |
|
Acceptance as self-expert: treat patient as competent expert of himself, respect individual framing and ability to take action |
Why do you think the two of you argue? |
|
Resource and future orientation: help patients to identify intra-psychic and interpersonal resources |
How can things get going again? Who can you and your family expect help from? |
|
NON-CONDUCIVE |
|
|
Command: utter advice, admonishment or orders |
The two of you should equally show each other respect and approach each other. |
|
Rationalization: to be one-sidedly logical, intellectual, oriented towards practical solutions and thereby disdaining emotions |
Meanwhile there are many studies and reference values. Talk to your doctor about the results, to be able to orientate yourself better. |
|
Projection/identification: transferring one's own experiences, thoughts and emotions on the patient |
I can understand your fear. I would feel as you do. |
|
Moralizing: to express moral judgment or evaluation |
Don't think of these things. It's important to think positive. |
|
Defense: to wander to other issues, to be indifferent, to defend emotions, to play down emotions, to be falsely resource-oriented |
Why should the operation go negatively? For us speech therapy is the important matter now. |
|
Generalization: inadequate generalizations, to play the individual off against the commonality |
Men are afraid of operations. |
|
Expert interpretation: to present hastily one's own explanations, interpretations or solutions as an expert, to interpret headstrong and subjectively, ask leading questions |
Due to your difficult situation you are under enormous stress. I think your wife understands that. |
|
Deficit orientation: answer focuses on deficits and pathologies |
Are you afraid not to wake up from narcosis again or that your illness is so bad that no operation is possible? |
|
OTHER |
|
|
Encouraging: abstract encouragement, disregarding patient's real resources |
Don't you lose courage! |
|
Being speechless/helpless |
I cannot tell you an exact prognosis. This is the doctor's job. |
|
Transferal to others |
Would you like to speak to a psychologist together with you wife? |
|
Offer help: therapist offers him/herself as help |
Please contact me whenever you need any help or support. If you wish, I'd be happy to visit the two of you at home. |
Table 6: Category system communication preferences
1) Patients with laryngeal tumors. <back>
2) "What experiences have you had with emotionally distressed tumor patients?" and "What difficulties have you experienced in dealing with them?" <back>
3) "Where do you see your strengths (weaknesses) in dealing with patients and their family members?" <back>
4) The distinction between active and passive knowledge was made because the current study also served to determine continuing education needs. For the subsequent planning of courses, it was important to distinguish whether mere (passive) knowledge or the practical/active use in exercises, role playing, etc. should gain greater attention. <back>
5) A tumor of the lower throat section. <back>
6) Tumor in the mouth. <back>
7) R = 2 x CÜ / (C1 + C2) (CÜ = number of agreeing codes, C1 and C2 number of codes of coder 1 and 2). The determination of reliability coefficients, as with Cohens Kappa, was not possible based on the possible multiple coding of text sequences. An Excel-add-in was used to calculate the inter-coder reliability for MAXQDA projects "IRPrüfung 2" by Michael LENZ (see http://www.mlenz.de/portal/fuer-maxqda.html). <back>
8) The indicated IDs correspond to the internal project numbers of the 33 interviewees. <back>
9) With the material we had, it was not possible to conduct an in-depth analysis of the backgrounds of this initially contradictory result at the individual level. <back>
10) The small number also results from a conservative coding. Many statements (for example, "I understand that very well") can both have an empathetic component and contain insufficient boundaries and projective or identifying moments. When this could not be conclusively reconstructed, the negative category was not assigned. <back>
11) If a discussion style is represented by three answer possibilities, then 100% = 84 (three answer possibilities x 28 people interviewed = 84, etc.). <back>
Archer, Jo; Hutchison, Iain & Korszun, Ania (2008). Mood and malignancy: Head and neck cancer and depression. Journal of Oral Pathology & Medicine, 37(5), 255-270.
Bortz, Jürgen & Döring, Nicola (2005). Forschungsmethoden und Evaluation für Human- und Sozialwissenschaftler. Heidelberg: Springer.
Fallowfield, Lesley (1995). Can we improve the professional and personal fulfillment of doctors in cancer medicine. British Journal of Cancer, 71(6), 1132-1133.
Fallowfield, Lesley; Jenkins, Valerie; Farewell, Vern; Saul, Jacky; Duffy, Anthony & Eves, Rebecca (2002). Efficacy of a cancer research UK communication skills training model for oncologists: A randomised controlled trial. Lancet, 359, 650-656.
Fogarty, Linda A.; Curbow, Barbara A.; Wingard, John R.; McDonnell, Karen & Somerfield, Mark R. (1999). Can 40 seconds of compassion reduce patient anxiety? Journal of Clinical Oncology, 17, 371-379.
Jenkins, Valerie & Fallowfield, Lesley (2002). Can communication skills training alter physicians beliefs and behavior in clinics? Journal of Clinical Oncology, 20, 765-769.
Kappauf, Herbert W. (2004). Kommunikation in der Onkologie. Der Onkologe, 11, 1251-1260.
Krauß, Oliver (2001). Konstruktion und Evaluation eines Trainingsprogramms zum Umgang mit Sterbenden und ihren Angehörigen. Dissertation, University of Leipzig, Faculty for Biology, Pharmacy and Psychology.
Langewitz, Wolf (2002). Arzt-Patient-Kommunikation, Mitteilen schlechter Nachrichten. In Elmar Brähler & Bernhard Strauss (Eds.), Handlungsfelder in der Psychosozialen Medizin (pp.54-76). Göttingen: Hogrefe.
Maguire, Peter (1999). Improving communication with cancer patients. European Journal of Cancer, 35, 1415-1422.
Maguire, Peter & Pitceathly, Carolyn (2002). Key communication skills and how to acquire them. British Medical Journal, 325, 697-700.
Massie, Mary J. (2004). Prevalence of depression in patients with cancer. Journal of the National Cancer Institute, 32, 57-71.
Mayring, Philipp (2000). Qualitative content analysis. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 1(2), Art. 20, http://nbn-resolving.de/urn:nbn:de:0114-fqs0002204.
Parle, Michael; Maguire, Peter & Heaven, Cathy (1997). The development of a training model to improve health professionals' skills, self-efficacy and outcome expectancies when communicating with cancer patients. Social Science and Medicine, 44, 231-240.
Razavi, Darius & Delvaux, Nicole (1997). Communication skills and psychological training in oncology. European Journal of Cancer, 33, S15-S21.
Roter, Debra L.; Hall, Judith A.; Kern, David E.; Barker, Lee R.; Cole, Karan A. & Roca, Robert P. (1995). Improving physicians interviewing skills and reducing patients emotional distress—a randomized clinical-trial. Archives of Internal Medicine, 155, 1877-1884.
Singer, Susanne; Bringmann, Holger; Hauss, Johann; Kortmann, Rolf Dieter; Kohler, Uwe; Krauß, Oliver & Schwarz, Reinhold (2007). Prevalence of concomitant psychiatric disorders and the desire for psychosocial help in patients with malignant tumors in an acute hospital. Deutsche Medizinische Wochenschrift, 132, 2071-2076.
Singer, Susanne; Danker, Helge; Dietz, Andreas; Hornemann, Beate; Koscielny, Sven; Oeken, Jens; Matthäus, Christoph; Vogel, Hans-Joachim & Krauß, Oliver (2008). Screening for mental disorders in laryngeal cancer patients: A comparison of 6 methods. Psycho-oncology, 17, 280-286.
Stiefel, Friedrich & Razavi, Darius (2006). Informing about diagnosis, relapse and progression of disease—communication with the terminally III cancer patient. Recent Results in Cancer Research, 168, 37-46.
Ullrich, Peter (2006). Das explorative ExpertInneninterview. Modifikation und konkrete Umsetzung der Auswertung von ExpertInneninterviews nach Meuser/Nagel. In Tim Engartner, Diana Kuring & Thorsten Teubl (Eds.), Die Transformation des Politischen. Analysen, Deutungen, Perspektiven (pp.100-109). Berlin: Karl-Dietz Verlag.
Ullrich, Peter (2010, in print). Kritik mit Methode? Sieben Thesen zum Verhältnis von Forschungsmethoden und Gesellschaftskritik. In Martin Dege, Till Grallert, Carmen Dege & Niklas Chimirri (Eds.), Möglichkeiten politischen Handelns in den Sozialwissenschaften. Gießen: Psychosozial.
van't Spijker, Adriaan, Trijsburg, R. Wim & Duivenvoorden, Hugo J. (1997). Psychological sequelae of cancer diagnosis: A meta-analytical review of 58 studies after 1980. Psychosomatic Medicine, 59, 280-293.
Wollbrück, Dorit & Danker, Helge (2006). Psychosozialer Kurs für onkologisch tätige Logopäden und Sprechwissenschaftler. Forum Logopädie, 6, 7.
Peter ULLRICH, PhD, is a cultural scientist/sociologist; his research interests are in political sociology (protest, social movements, surveillance, anti-Semitism, anti-Zionism, Middle-East-conflict) and medical sociology (prevention and governmentality, health services research).
Contact:
Peter Ullrich
Department of Medical Psychology and Medical Sociology
University of Leipzig
Philipp-Rosenthal-Str. 55
D-04103 Leipzig, Germany
Tel.: +49 341 9715438
Fax: +49 341 9718809
E-mail: Peter.Ullrich@medizin.uni-leipzig.de
URL: http://peterullrich.twoday.net, http://medpsy.uniklinikum-leipzig.de/ullrich.html
Dorit WOLLBRÜCK, Dipl.-Psych. (psychologist), conducts research mainly in psychosocial oncology and psychooncological further training.
Contact:
Dorit Wollbrück
Department of Medical Psychology and Medical Sociology
University of Leipzig
Philipp-Rosenthal-Str. 55
D-04103 Leipzig, Germany
Tel.: +49 341 9715458
Fax: +49 341 9718809
E-mail: dorit.wollbrueck@medizin.uni-leipzig.de
URL: http://medpsy.uniklinikum-leipzig.de/
Helge DANKER, Dipl.-Psych. (psychologist), conducts research in psychooncology, psychosocial aspects of head and neck cancer and psychological counseling in oncology.
Contact:
Helge Danker
Department of Medical Psychology and Medical Sociology
University of Leipzig
Philipp-Rosenthal-Str. 55
D-04103 Leipzig, Germany
Tel.: +49 341 9715427
Fax: +49 341 9718809
E-mail: helge.danker@medizin.uni-leipzig.de
URL: http://medpsy.uniklinikum-leipzig.de/
Susanne KUHNT, Dipl.-Psych (psychologist), is a communication coach; her area of expertise is psycho-oncology; she specializes in communication, cancer related fatigue, cancer related distress, evaluation of psychosocial counseling services for cancer patients.
Contact:
Susanne Kuhnt
Department of Medical Psychology and Medical Sociology
University of Leipzig
Philipp-Rosenthal-Str. 55
D-04103 Leipzig, Germany
Tel.: +49 341 9715458
Fax: +49 341 9718809
E-mail: susanne.kuhnt@medizin.uni-leipzig.de
URL: http://medpsy.uniklinikum-leipzig.de/
Elmar BRÄHLER, Prof. Dr. rer. biol. hum. habil., is Head of the Department of Medical Psychology and Medical Sociology and conducts research in psychodiagnosis, psychological aspects of fertility problems, coping with chronic illnesses, health/illness and gender, health identity of immigrants, medical-ethical questions in reproductive medicine, unemployment and health, right-wing extremism and psycho-oncology.
Contact:
Elmar Brähler
Department of Medical Psychology and Medical Sociology
University of Leipzig
Philipp-Rosenthal-Str. 55
D-04103 Leipzig, Germany
Tel.: +49 3419718801
Fax: +49 341 9718809
E-mail: elmar.braehler@medizin.uni-leipzig.de
URL: http://medpsy.uniklinikum-leipzig.de/
Susanne SINGER, Dr. rer. med., Dipl.-Psych. (psychologist), MSc Epidemiology; she conducts research in psychosocial oncology (especially psycho-oncology in laryngorhinootology, psychological comorbidity, quality of life) and salutogenesis.
Contact:
Susanne Singer
Department of Medical Psychology and Medical Sociology
University of Leipzig
Philipp-Rosenthal-Str. 55
D-04103 Leipzig, Germany
Tel.: +49 341 9715463
Fax: +49 341 9718809
E-mail: susanne.singer@medizin.uni-leipzig.de
URL: http://medpsy.uniklinikum-leipzig.de/
Ullrich, Peter; Wollbrück, Dorit; Danker, Helge; Kuhnt, Susanne; Brähler, Elmar & Singer, Susanne (2010). Psychosocial Aspects of Speech Therapy with Head and Neck Cancer Patients: Clinical Experiences, Communicative Skills and the Need to Train Speech Therapists in Oncology [71 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 11(1), Art. 22, http://nbn-resolving.de/urn:nbn:de:0114-fqs1001220.