

Volume 8, No. 1, Art. 17 – January 2007
"Natural", "Normal": Discourse and Practice at St. Bartholomew's Hospital, London, and Addenbrooke's Hospital, Cambridge, 1880-1920
Rosemary Wall
Abstract: Elite physicians have been portrayed as opposed to the use of laboratory science in the hospital. In this paper John Harley WARNER's research regarding use of the terms "natural" and "normal" in case notes in the U.S., as representative of the growing influence of laboratory science in the hospital, is compared to use of these words at St. Bartholomew's Hospital, London, and Addenbrooke's Hospital, Cambridge, England. Discourse at Bart's appears to support the view of elite opposition to the laboratory. However, the case notes reveal that the bacteriological laboratory was used at least as often as at Addenbrooke's. This apparent contradiction is investigated by examining how the words "natural" and "normal" were used, and the reception of experimental physiology at the hospitals. Samuel GEE, a physician at Bart's in the late nineteenth century, who also, at first glance, had contradictory views on the use of the laboratory in the hospital, is examined through his practice and writings in order to understand that representations of reception of laboratory science are not straightforward. Analysing changes in language over time shows that rhetoric and practice are not always aligned, and that language cannot always be seen as an indicator of the latter.
Key words: discourse, bacteriology, experimental physiology, laboratory, hospital, St. Bartholomew's Hospital London, Addenbrooke's Hospital Cambridge, England, Samuel Gee
Table of Contents
1. Introduction
2. St. Bartholomew's Hospital—An Elite London Institution
3. Addenbrooke's Hospital, Cambridge—Unofficial Teaching Hospital to a Medieval University
4. Life on the Wards
5. Science and Standardisation: Exploring the Mindset of the Gentlemen Physicians
6. Experimental Physiology and Bacteriology—The Laboratory and Clinical Practice
7. Double Lives?—Samuel GEE
8. Conclusion
Elite London physicians have presented themselves as both opposed to laboratory science and specialisation, and as embracing these new developments in the age of the rise of laboratory biomedical sciences. Current historiography has concentrated on the former representation of these elite physicians, portraying them as considering medicine an art rather than a science. This case has especially been put forward for the physicians at St. Bartholomew's Hospital in London1). An analysis of discourse in the case notes from Bart's between 1880 and 1920 appears to confirm the idea that physicians were reluctant to fully support the changes in ideology that experimental laboratory science brought to medicine. This is especially highlighted when Bart's is compared to Addenbrooke's Hospital, at the time the unofficial teaching hospital for the University of Cambridge, and to hospitals in the United States of America. However, the idea that elite physicians were not opposed to the laboratory has recently been raised regarding the practice of elite physicians who used commercial bacteriological laboratories, as only elite practitioners with wealthy patients could have afforded the prices charged by these institutions (WORBOYS, 2004). Looking at medical practice at Bart's confirms this view, and shows that the elite physicians who worked there welcomed the new science of bacteriology. [1]
The understanding of discourse in this paper is informed by work on the U.S.. One of the major findings in John Harley WARNER's (1997a) pioneering study of patient records is the change of language from "natural" to "normal" over time. He shows, with examples of two U.S. hospitals, that the use of the word "natural" to describe a state of well-being had been "almost completely replaced" by "normal" by the mid-1870s. "Natural" related to an individual's well-being, which could differ with the seasons, or with ethnicity, location or sex, for example (WARNER, 1997a, pp.85-86). The term "natural" refers to disease as non-specific, and as "systemic imbalances in the body's natural harmony" (WARNER, 1997a, p.86)2). "Normal" is a word from experimental physiology which belongs to the second half of the nineteenth century, when "universalized norms defined by laboratory science" became the way to consider well-being (WARNER, 1997a, pp.86-87). This is reflected in the graphical and quantitative representation of temperature, pulse, respiration and urinalysis—matching measurements to "normal standards" (WARNER, 1997a, p.87). Machines used in experimental physiology such as the kymograph recorded graphical images of the pulse or the respiration of an animal, and this recording of information in a graphical form took off in clinical medicine. [2]
The main sources for this study are clinical case notes from Bart's and Addenbrooke's Hospitals in order to compare use of language with use of bacteriological methods of diagnosis. As a sampling method, all of the existing case notes for pulmonary tuberculosis, typhoid fever and diphtheria have been examined from the years between 1880 and 19203). This paper challenges the existing secondary literature in the field of history by using sources depicting what actually happened, written at the time of these everyday events. Discourse can help to reveal the mindset of the physicians, and whether they were ready for the appropriation of laboratory science, and how much they believed in the worth of its techniques and products. [3]
There will be slightly more focus on Bart's in this paper, as this is the hospital which shall be shown to not fit with the pattern of the clear transition through time from the use of the word "natural" to the word "normal". In order to examine the differences between the hospitals I shall first examine how Bart's and Addenbrooke's have been represented by historians. The creation of case notes at each hospital shall be considered, and then the use of language at both of the English hospitals will be compared with use of language in the U.S. Differences will be considered in light of the use of laboratory sciences at the two English hospitals, and the "double lives" which Bart's physicians appeared to lead, focusing on Samuel GEE as an example of the latter. [4]
Although being linked by the theme "Time and Discourse" to the other papers in this volume, this contribution is different in that it looks at change in discourse over a long time period of forty years. Also, it looks at the late nineteenth and early twentieth centuries whereas the other papers examine contemporary events or the very recent past. However, MOREIRA and especially MOTZKAU, ground their work historically. The paper also differs from almost all of the others by examining the use of particular words to examine changing concepts, rather than a wider framework of discourse. The use of these words is, however, analysed to examine the more general change in ideology regarding the use of laboratory science in medicine. There are similarities to ELGAARD JENSEN's paper, which looks at a single word in examining the construction of the "future" in discourse in a study of representation of a new kind of office space, analysing how this word is used to persuade "witnesses" and how it is then replicated. The identity of the company is constructed through this word, and in this paper on the history of medicine, words are also seen to illustrate a changing identity of physicians over time. Although this paper considers the discourse of a hundred years ago, one of the main sources for this work overlaps with that used by other studies in this volume which partly focus on documents and their creation to empirically examine time and discourse, such as those by KONTOPODIS and ELGAARD JENSEN. Unfortunately, although there are surviving memoirs and private papers, it is not as possible to determine the creation of these century-old documents with as much accuracy as scholars of contemporary workplace activities. [5]
2. St. Bartholomew's Hospital—An Elite London Institution
St. Bartholomew's Hospital is the oldest continually open hospital in Britain, and perhaps was the most prestigious in the country between 1880 and 1920. Historian of medicine, Christopher LAWRENCE, focuses on the physicians at this hospital, especially in his article on the interwar years (LAWRENCE, 1998), giving the impression that at this hospital the physicians would not have routinely used a diagnostic laboratory with specialist pathologists diagnosing patients away from the bedside (LAWRENCE, 1985; 1998; 1999; 2000). [6]
Roy PORTER, Jeanne PETERSON and Christopher LAWRENCE have all examined how London hospital physicians differed from those in the rest of the country, except perhaps Oxford. Roy PORTER (2001, p.255) describes London's elite physicians of the nineteenth century as having "plush positions of professional authority and eminence." One of Christopher LAWRENCE's (1985; 1998) main themes in his articles on the London medical profession and their clinical practice from 1850-1939, is the idea of gentility amongst the elite. He attributes this mentality to the "distinguished lay governors" who selected physicians by "class attributes rather than medical skill"; the importance of "character more than the pursuit of expertise" (LAWRENCE, 1985, pp.503-504). Elite London physicians also controlled the professional institutions, holding the highest offices of the Royal College of Physicians and Surgeons (PETERSON, 1978, p.137). Jeanne PETERSON (1978, p.136) perhaps best sums up the status of these physicians:
"Those who practiced in London hospitals and in private practice were rewarded with high social connections, prosperity if not wealth, and … [the] pleasures of the upper ranks of Victorian society. Knighthoods or baronetcies, country houses, lavish entertaining, foreign travel, Alpine mountain-climbing, membership at the Athenaeum, art collecting—all were possible for the select few who were numbered among the London medical and surgical elite. They often married well, sent their sons to public school and university; they owned carriages, hired servants, and donned the morning coats and top hats that daily bespoke their elevated status." [7]
In the 1960s, the London teaching hospitals were "still the seats of power", in the words of commentator Paul FERRIS (1965, pp.61-62), especially St. Bartholomew's Hospital and St. Thomas's Hospital, which had the "best social standing and the nicest upper-class nurses." [8]
Despite the eminence of the London teaching hospitals, they have not been seen as the most progressive of hospitals in their use of scientific knowledge and medical technology by some historians and commentators. According to LAWRENCE (1985, p.507), for gentlemen physicians clinical medicine was "based on science" but was an "art which necessitated that its practitioners be the most cultured of men and the most experienced reflectors on the human condition." He examines the delayed use of medical instruments such as the sphygmograph and sphygmomanometer, as described in published medical literature (LAWRENCE, 1985, pp.515-516). The gentlemen physicians of the interwar years were apparently "anti-mechanization and standardization" due to their holistic worldview (LAWRENCE, 1998, p.94). The London teaching hospitals of the 1960s were still "stiff with protocol, old-fashioned and due to lose their grip on the central mysteries of medicine" (FERRIS, 1965, p.62). FERRIS (1965, p.64) wrote:
"Medicine as a whole is becoming so complex that the individual performer will soon seem an archaic figure, mumbling the magic formula, 'bedside medicine,' obsessed with the gentlemanliness of his profession. But the London system is still rooted in this archaic individualism of the part-time gentleman." [9]
LAWRENCE (1998, p.95) considers that the interwar gentlemen physicians approved of the laboratory for diagnostic and experimental purposes but "were determined to integrate it into their preferred social order"—an order which opposed specialisation. Apparently, physicians like St. Bartholomew's Thomas HORDER believed that all clinical pathology should be carried out by the clinician himself, and Sir Walter LANGDON-BROWN worried about the division of labour in society in general (LAWRENCE, 1998, pp.98 and 105). Joel D. HOWELL (1987, p.58), who has examined the use of technology in the hospital in the U.S., considers that in the early twentieth century, British physicians as a whole did not accept "[t]he bacteriologist and his gram stains; the physiologist and his kymograph" as part of "normal" clinical medicine, and that these techniques were for "training purposes in an academic setting." Apparently specialisation in medicine was also not accepted throughout the country (HOWELL, 1987, p.59). This appears to be the current prevailing view in the secondary literature, and partly so in the physicians' published primary literature. [10]
3. Addenbrooke's Hospital, Cambridge—Unofficial Teaching Hospital to a Medieval University
At the beginning of the period of this study, the University of Cambridge's department of Medicine was developing a reputation to rival the London medical schools. The status of the school had been very low in the early nineteenth century. From 1833 to 1858 an average of less than four students per year studied Medicine at the University, and the qualification obtained was not highly regarded within the medical profession (ROOK, CARLTON & CANNON, 1991, pp.118-119). Medical journals compared Cambridge unfavourably with the London medical schools with regard to size of hospitals and lack of dissecting rooms (WEATHERALL, 2000, p.15). However, bedside clinical instruction had been given to Cambridge medical students from 1819 (WEATHERALL, 2000, p.63). By the late nineteenth century the reputation of the school had changed with 70 students joining the medical course in 1880 (WEATHERALL, 2000, p.110) and Cambridge having one of the largest medical schools in the country by 1891. At this time the degree was regarded as "one of the highest professional qualifications" (ROOK et al., 1991, pp.118-119). However, Addenbrooke's Hospital continued to be too small to cope with all the medical students for their whole degree, so London hospitals, amongst others, were used for student placements during the late nineteenth century (WEATHERALL, 2000, p.131). According to WEATHERALL (2000, p.116), the aim of the Cambridge medical school was to attract physicians who had "clinical ability and scientific curiosity"—people like John BRADBURY who was Physician to Addenbrooke's for fifty years and who also published on pathological and clinical subjects in the BMJ and the Lancet. Cambridge is also an interesting case to study in comparison to Bart's, as Gerald GEISON (1978, pp.9, 81 and 96) considers that Cambridge was a university in transition from the 1870s. University professors were taking their jobs more seriously, considering an academic career could be for life, and both transmitting and producing knowledge. He demonstrates this changing environment by linking the growth of Michael FOSTER's physiological school with that of the rise of the Cavendish Laboratory for physics. He considers that without this change at Cambridge, English physiology would have been very different (GEISON, 1978, p.47). In suggesting that biology in Cambridge would have been transformed by George HUMPHRY, the surgeon, if FOSTER had not come to Cambridge, GEISON (1978, p.123) shows that he considers that the town and university were perhaps more important than the person. Therefore, the general milieu in Cambridge in the late nineteenth century with regard to laboratory science is very important to consider when examining changing discourse and practice. [11]
The connection between the University of Cambridge and Addenbrooke's Hospital appeared assured as, from 1785, it had been the tradition that a physician at Addenbrooke's Hospital was appointed the Regius Professor of Physic at Cambridge (ROOK et al., 1991, p.238)4). Other physicians at the hospital included Downing Professors of Medicine, Fellows of various colleges and one Lucasian Professor of Mathematics (ROOK et al., pp.60, 61, 83, 85, 101). However, when Clifford ALLBUTT (a supporter of the value of experimental science for the practice of medicine) was appointed as the Regius Professor in 1892, this relationship came into question. Clifford ALLBUTT was, according to Sir Walter LANGDON-BROWN, appointed as it was too hard to choose between the three physicians at Addenbrooke's (ROOK et al., 1991, p.238)5). ALLBUTT was not to receive a position at the Hospital until 1900, although he did deputise for Dr Donald MACALISTER in the summers of 1896-97 (ROOK et al., 1991, p.247). In 1895, the Vice Chancellor asked the Hospital for a conference to establish "a closer and more regular connexion between the Hospital and the University Teachers in the Department of Medicine." All members of staff at the Hospital, except one, were also professors or teachers at the university, and clinical lectures were given in the wards, the Board Room, and the Operating Theatre, but there was still no official link (ROOK et al., 1991, pp.238-239). In 1896, it was agreed in the Committee that Lecturers could use the hospital, and its patients, for teaching purposes, but not alter patients' treatment. In 1900, it was agreed that the University would pay the hospital £300 per year, and the Regius Professor could be a Physician, with the Professor choosing whether he would like beds to supervise, or whether he would only like them for teaching purposes. ALLBUTT declined the offer of beds to supervise, telling the Hospital he already had enough for teaching purposes (ROOK et al., 1991, p.248). He did not take over the care of any beds until staff shortages during the First World War (ROOK et al., 1991, p.315). However, the links between the hospital and the university were also practical in the nature of diagnosis of patients. Addenbrooke's' X-rays were initially carried out at the Cavendish Laboratory, by members of staff there—Mr. W.H. HAYLES and Mr. EVERETT—as early as 1896. Indeed, Mr. HAYLES was, according to some Cambridge medical historians, probably the "first man in England to take an X-ray" (ROOK et al., 1991, p.332). Addenbrooke's got its own machine in 1903, firstly with surgeons unsuccessfully taking their own photographs, and subsequently in 1907 with Mr. FIELD, the dispenser, learning how to use it from staff at Bart's. This is interesting considering the view discussed earlier of Bart's and technological instruments (ROOK et al., 1991, p.332). The Hospital and University were also closely connected in geographical terms. In the late nineteenth century, Addenbrooke's Hospital and the New Museums site, which began construction in 1863, were closely situated in Cambridge (WEATHERALL, 2000, p.98). The location of the Cavendish Laboratory on Free School Lane would have enabled close interaction between Hospital and University.
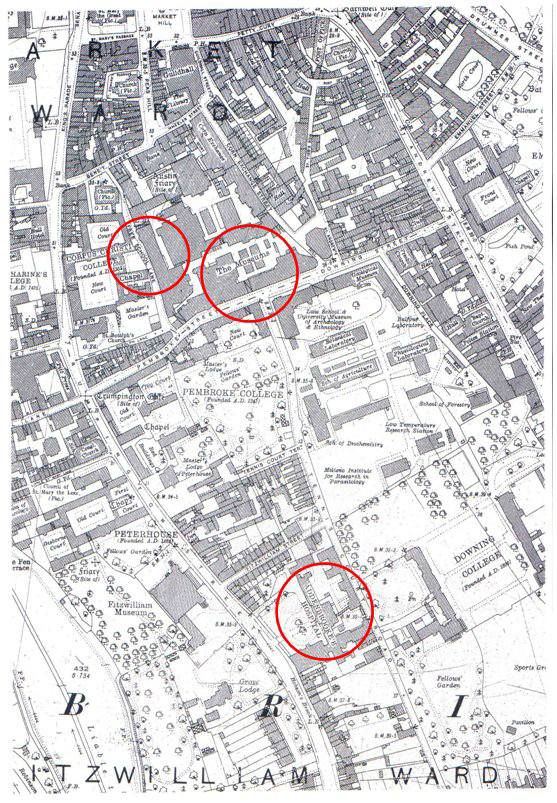
Illustration 1: Map of Cambridge—Laboratories and Hospital Area (CAMBRIDGE PARLIAMENTARY AND MUNICIPAL BOROUGH, 1927) [12]
The University also had political control over the Hospital even though an official connection was lacking. Scientists at the University of Cambridge gained more importance in decision- making in the latter quarter of the nineteenth century. In 1878, George PAGET, Regius Professor of Physic, complained about the lack of consultation in the proposed election of a professor for physiology at Trinity College and how this typified the importance given to natural sciences compared to medicine (GEISON, 1978, p.108)6). In 1883-4, the scientists at the University were officially given more power than the physicians who had positions at the University. A university-wide decision was made to give more power in decision-making to residents of the University, as opposed to non-residents. This meant that the Board of Medicine came to have a clear majority of pre-clinical scientists, and led to the first Professor of Pathology, Charles Smart ROY, being a physiological pathologist, rather than a clinical pathologist (WEATHERALL, 2000, pp.133 and 139)7). The Lancet announced at the news of this appointment that it would "blight the hopes of those who were looking forward to the establishment of a practical medicine school at Cambridge" for ROY was really an experimental physiologist (WEATHERALL, 2000, p.143)8). GEISON (1978, pp.365-366) considers that FOSTER had a key part to play in the appointment of Clifford ALLBUTT. This loss of control of Medicine in the University angered the physicians at Addenbrooke's and perhaps contributed to the delay in ALLBUTT being accepted at the Hospital (WEATHERALL, 2000, p.189). [13]
From the clinical records at Bart's it is clear that the internal medicine case notes were not actually completed by the physicians examined in this paper, but by clinical clerks. Their names always begin with "Mr." rather than "Dr." in the internal medicine case notes. However, there are indicators that the physicians had a heavy influence on the case notes. Geoffrey BOURNE (1963, pp.35 and 123), a student and subsequently physician at Bart's, has written an autobiography which tells in detail the procedures followed. The "Clinical Clerks" mentioned in the case notes were medical students in the clinical years of their degree. Clerking involved taking histories and physical examinations. Physicians were involved in this process though. BOURNE describes how John DRYSDALE led students to describe the condition of the patient through his "Socratic method of careful questioning", and then led them through "examination, inspection, palpation, percussion and auscultation." These notes were read out to the consultants and were criticised by them as to length, content, and style of writing and language (BOURNE, 1963, pp.36-37 and 78). [14]
In a couple of instances in the casebooks, physicians' involvement is illustrated. For example, physicians signed requests for the pathologist to undertake a Widal's test (invented in 1896). This is in the same case book, in 1898, but signed by two different doctors—CHURCH and MOORE (SBH 16/41/141; 16/41/181). There are common characteristics in case notes supervised by the same clinician, such as this symbol which was only used in two case books of DUCKWORTH's:

Illustration 2: Symbol for Typhoid [15]
The symbol was used frequently in 1893 (in five out of ten cases) and in 1897 (in two out of four cases). The phrase "Typhoides Febris" was only used under the care of Dr. TOOTH for all three cases examined on his ward in 1911 and 1913 (SBH 16/39 and 16/43). This again shows the influence of physicians on their clerks' notes, as it happened over three years. It seems, judging by handwriting, that Samuel GEE wrote part or all of 69 out of 90 sets of case notes between 1882 and 18999). [16]
The case notes for Addenbrooke's Hospital are not uniform like those at Bart's. Case notes from Bart's are almost always complete and include in order a front sheet with the patient's personal details and a summary of the case and usually a diagnosis, the notes taken during the patient's stay, graphs documenting temperature with accompanying charts with information about urinalysis, for example, and a sheet detailing diet and treatments prescribed. Later, extra pages such as pathology and X-ray reports were included. These are not in specific places in the notes. Addenbrooke's case notes contain similar sources of information, but on many occasions they are not all present. Addenbrooke's case notes are signed by "House physicians" rather than "clinical clerks". It appears that either standards and expectations of completion of case notes were much higher at Bart's, or that students were more conscientious than junior doctors when completing case notes in order to impress their teachers and pass their degree. The influence which physicians had on students' notes at Bart's may mean they show a previous generation's views when compared to notes compiled by junior doctors at Addenbrooke's. [17]
5. Science and Standardisation: Exploring the Mindset of the Gentlemen Physicians
WARNER shows the transition from "natural" to "normal" with his study of the records of the Massachusetts General Hospital and the Commercial Hospital of Cincinnati. WARNER's (1997a, pp.104 and 113) sample of cases—about 4000—compared to the 405 cases examined at Bart's and 1418 at Addenbrooke's is more significant for trends. However, there are noticeable differences which can be seen between St. Bartholomew's Hospital and the two hospitals in the U.S.. Illustration 3 shows the percentages of cases in which WARNER found these two words at each hospital.
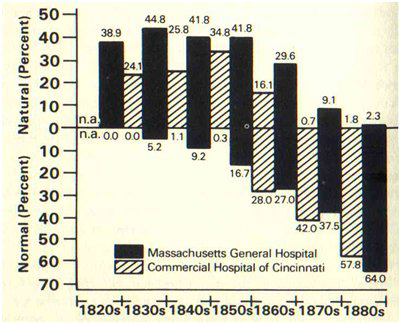
Illustration 3: Percentage of case notes in which terms "natural" and "normal" appear, from WARNER (1997a, p.88) [18]
The change is significant with hardly any records using "natural" by the 1870s and 1880s at both hospitals. Illustration 4 shows the percentages of cases using "natural" and "normal" each year at Bart's.
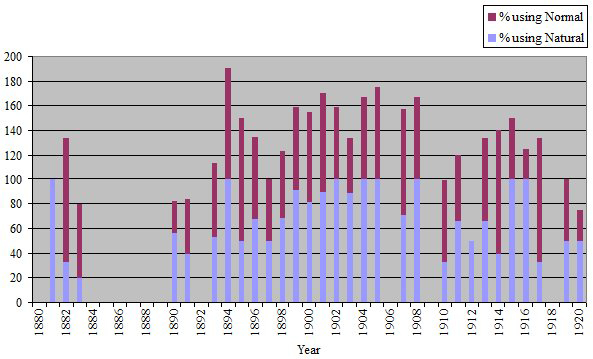
Illustration 4: Percentage of the sample of case notes from St. Bartholomew's Hospital which use the terms "natural" and "normal"
[19]
An entirely different picture is shown. The period represented by Illustration 4 begins where WARNER's ends, but shows that "natural" was still commonly used right up until 1920, with "normal" not even becoming predominant by the last years of the four decades shown. As "natural" and "normal" were used concurrently at Bart's, this way of representing data is not perhaps the most profitable.
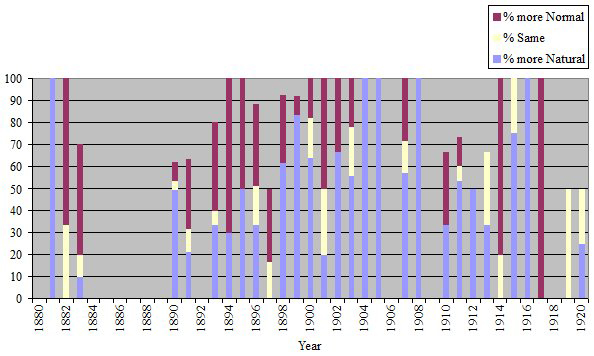
Illustration 5: Percentage of the sample of case notes from St. Bartholomew's Hospital in which "natural" or "normal" are
used more than the other [20]
Illustration 5 shows the percentages of cases in which either "natural" or "normal" were used the most, revealing that "natural" was more predominant in use than "normal" throughout most of the period. WARNER considers that the use of language in medical records reflects the change in "cognition" of the physicians. Although the sample is small compared to WARNER's, the word natural was evidently very much in use at Bart's throughout the period 1880-1920, indicating that medical practice would, like language, not be affected as much as other hospitals by new scientific knowledge produced in the laboratory. [21]
At Addenbrooke's, as would be expected with the influences the hospital had from the University of Cambridge, "normal" superseded "natural" from an early stage, as shown in Illustrations 6 and 7.
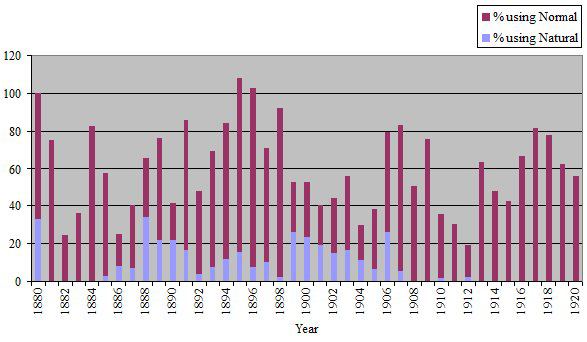
Illustration 6: Percentage of the sample of case notes from Addenbrooke's Hospital which use the terms "natural" and "normal"
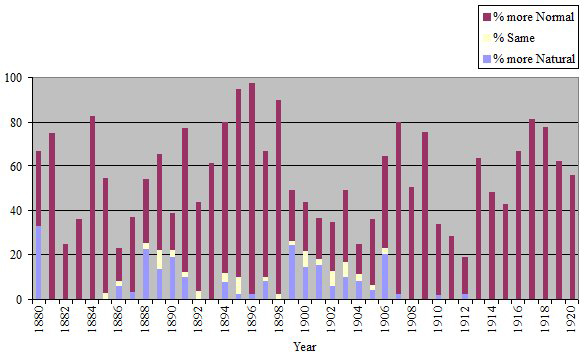
Illustration 7: Percentage of the sample of case notes from Addenbrooke's Hospital in which "natural" and "normal" are used
more than the other [22]
"Natural" and "normal" were often written close together in case notes, even for the same types of descriptions. For example, in an Addenbrooke's' case note it was written in 1902, "Cor. natural and in normal position" (AH 025/8-9/208). A Bart's' case note states in 1896, "Knee jerks nat." and then in the same handwriting the next day, with only two lines in between, it was written, "Knee jerks normal" (SBH 16/042/028). This could be used to question the change in use of "natural" and "normal," especially for Bart's where both terms were used commonly until 1920. However, often the way in which both terms were used in the same case note was when there was a reference to the temperature being normal. WARNER (1997a, pp.89-90) found in U.S. case notes that quantitative measurements were described as "normal" before qualitative descriptions. This was especially the case for evidence gained using instruments such as the "stethoscope, thermometer, or time-piece". [23]
Illustration 8 shows the proportion of case notes in which temperature is referred to as either "natural" or "normal". As I have counted the total number of times each term is used in each case note, the result is sometimes above one hundred per cent—therefore this is a relative representation of the use of "natural" and "normal" using case notes as a base comparison number. It can clearly be seen that temperature was nearly always referred to as "normal" at Bart's.
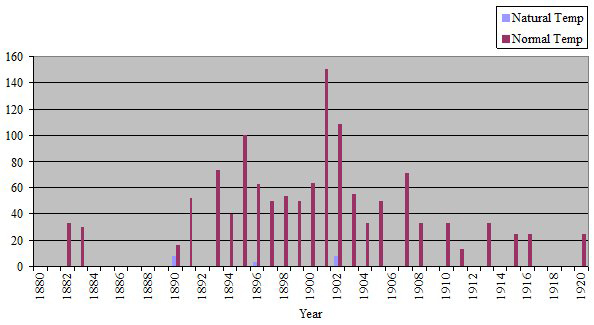
Illustration 8: Percentage of the sample of case notes from St. Bartholomew's Hospital in which temperature is referred to
as either "natural" or "normal" (case notes as base number to judge percentage) [24]
At Addenbrooke's temperature was never referred to as "natural" in the sample case notes. This use of the term "normal" for a quantitative measure correlates with WARNER's study. However, Bart's does not follow the same pattern when heart sounds are examined (Illustration 9):
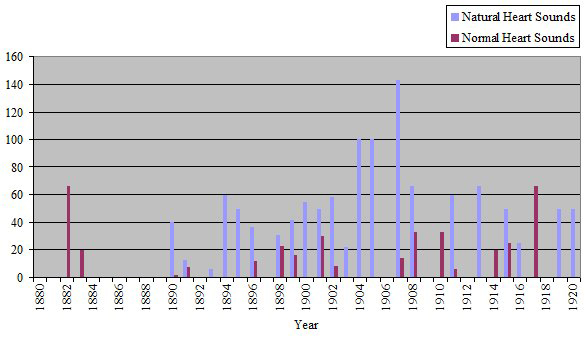
Illustration 9: Percentage of the sample of case notes from St. Bartholomew's Hospital in which heart sounds are referred to as either "natural" or "normal" (case notes as base number to judge percentage) [25]
However, at Addenbrooke's doctors used predominantly "normal" to describe heart sounds, right from the beginning of the period, and exclusively so from 1907. Therefore, the relationship between language and possibly quantitative measures at Bart's is not simple. However, surely temperature is easier to consider as "normal" than heart sounds, as there was a set figure in the graphs in the case notes determined as normal, with a printed line drawn across at that point. [26]
The way in which a qualitative, subjective description of organs or parts of the body (such as shape, position, what was palpable) was made demonstrates that Bart's staff and students used "natural" for this type of assessment (Illustration 10):
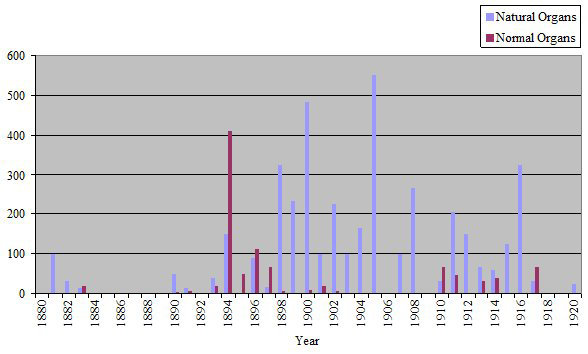
Illustration 10: Percentage of the sample of case notes from St. Bartholomew's Hospital in which subjective descriptions of
organs and parts of the body are referred to as either "natural" or "normal" (case notes as base number to judge percentage)
[27]
Addenbrooke's closely followed the American model even for this kind of description (Illustration 11):
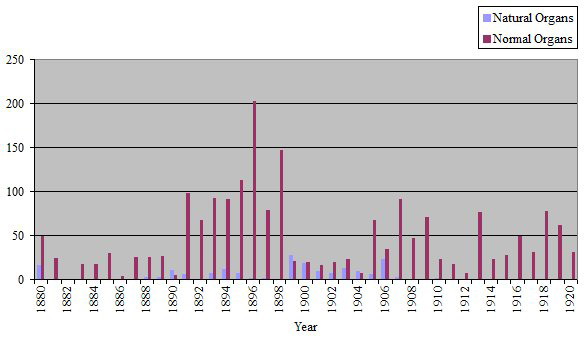
Illustration 11: Percentage of the sample of case notes from Addenbrooke's Hospital in which subjective descriptions of organs
and parts of the body are referred to as either "natural" or "normal" (case notes as base number to judge percentage) [28]
This analysis of the way in which "natural" and "normal" were used in general, and in particular contexts shows stark differences between the two hospitals investigated. Therefore the rest of the paper examines how laboratory science was perceived at the two hospitals in order to try to understand these differences. [29]
6. Experimental Physiology and Bacteriology—The Laboratory and Clinical Practice
WARNER (1997a, pp.5-6, 85-7) framed the change from "natural" to "normal" as coinciding with the gradual growth of experimental physiology as a model science for medicine. The use of therapeutics changed from acting on the body as a whole to restore the patient's individual "natural" balance, to working on specific parts of the body in line with knowledge gained from experimental physiology, with the aim of returning the body to universalised "measured, quantified norms" determined or influenced by the laboratory. The influence of experimental physiology may point to why changes in language were so different at Addenbrooke's than at Bart's. [30]
Mid to late nineteenth century German experimental physiology is associated with "biophysics" and the use of instruments (and also chemistry), sometimes resulting in graphical representation such as the recording of the pulse by the kymograph and sphygmograph (CRANEFIELD, 1957, p.407; FRANK, 1988, pp.215-16). This influence can clearly be seen in the case notes of the two English hospitals, where it is unusual for there to not be a graph in each case file showing temperature in the period examined in this paper. Chemical assaying, of urine for example, also showed the influence of chemical physiology. By the late nineteenth century, the University of Cambridge was arguably the "leading center of physiological research in England, if not the world" (GEISON, 1978, pp.183-4). The style of experimental physiology was not perhaps as exacting as in Germany, with less emphasis on graphical representation, and more on the senses. In 1874, however, FOSTER did receive money for recording apparatus for his laboratory which GEISON (1978, p.106) speculates was a kymograph. GASKELL, one of Foster's protégés, spent a year working with LUDWIG in 1874, the man who chiefly created the kymograph, and other students from Cambridge spent time in German laboratories (GEISON, 1978, pp.180-3 and 253). GEISON (1978, pp.253-6) discusses GASKELL's work on vaso-motor action and its continuation on his return to Cambridge, comparing the "Leipzig method" with the "Cambridge method". In Leipzig, under LUDWIG, GASKELL had conducted experiments using a larger dog, and the kymograph for measurement of blood flow, whereas in Cambridge he used the smaller frog ("as if in imitation of his smaller and less elaborate surroundings") and used the "Cambridge method" of a micrometer eyepiece for direct measurement of arterial diameters. GASKELL did later use the kymograph in Cambridge, though, in an experiment on the heart of a tortoise in 1883 (GEISON, 1978, p.295). However, the importance of experimental physiology in general and the numbers of students educated in its methods may have had an impact on the use of vocabulary at Addenbrooke's Hospital. Huge numbers of students studied elementary physiology, with an intake of 130 in 1885, and 190 in 1889 (GEISON, 1978, pp.306 and 308). FOSTER, HUMPHRY, and ALLBUTT at Cambridge thought it was preferable to the old system of students going straight from the mathematical tripos to clinical studies, for students to have training in pre-clinical natural sciences, with FOSTER thinking they should undertake the natural sciences tripos including physiology (GEISON, 1978, pp.365-6). [31]
Practical physiology teaching in England began in the late 1860s, with FOSTER's elective course at University College London (GEISON, 1978, p.330). England in general did not at all compete with German "biophysics". FOSTER remembered his mentor, William SHARPEY, at University College London, having to use a cylinder hat to explain the kymograph in the 1850s (GEISON, 1978, p.56). In 1870 the Royal College of Surgeons introduced a requirement that thirty classes of "practical" anatomy and physiology should be a requirement of the licentiate, with students themselves partaking in experiments, and the University of London adopted this requirement in 1871 (GEISON, 1978, pp.329). GEISON considers this development led to the growth of physiology in Britain (GEISON, 1978, pp.150-1). The discipline of physiology in Britain as a whole expanded between 1870 and 1900, at least arresting the flow of physiologists to the Continent (GEISON, 1978, p.150). [32]
Keir WADDINGTON (2003, pp.125-6) has presented physiology at Bart's as being taught reluctantly10). However, many of the initial problems which physiology faced were also present in Cambridge, such as lack of space for students (GEISON, 1978, pp.171-2). Although Bart's did not have the reputation of the Cambridge school of physiology, Thomas Lauder BRUNTON was very enthusiastic about experimental pharmacology and physiology, publishing widely, and working on treatments which had practical applications such as the action of digitalis. Like contemporaries at Cambridge, he spent time at the University College London laboratories, and in laboratories in Vienna, Berlin and at LUDWIG's laboratory in Leipzig in the early 1870s. However, rather than specialising in experimental physiology like GASKELL, he combined research with hospital medicine (WHITE FRANKLIN, 1974, pp.180-83; LAWRENCE, 1985, pp.516-17). Therefore, the impact of physiology at Bart's is not straightforward and requires further investigation, but no doubt did not have the same influence on medical practice as the famous laboratory at Cambridge. [33]
Bacteriology, and its forerunners from the 1840s (ideas of "specific chemical, fungal, and animalcular causes of disease"), also had an effect on ideas of universalised and specific disease causation (WARNER, 1997a, p.87). Examining use of bacteriological laboratory techniques shows different pictures of the reception of experimental science at Bart's and Addenbrooke's. [34]
Contrary to use of language, bacteriological methods can be shown to have been accepted slightly more enthusiastically at Bart's than at Addenbrooke's. For typhoid fever, the diagnostic Widal's test was discovered in 1896. This agglutination test was widely used from 1898 at Bart's, with it being documented in all of the eight surviving case notes from 1898, and thereafter regularly used in surviving case files, only for one year in 1902 dropping below 60 per cent of cases. The bacteriological test for pulmonary tuberculosis, of looking for tubercle bacilli in sputa, was not used as routinely as the test for typhoid, though it was still used regularly. It was probably not used as often due to fairly effective existing methods of percussion and auscultation. The most convincing of the sample diseases for illustrating routine use of the bacteriological laboratory at Bart's is diphtheria. There was a slow acceptance of the bacteriological examination for diphtheria (the bacillus was isolated in 1883) due to widely acknowledged problems with reliability and staining (HAMMONDS, 1999, pp.50-52; ANDREWES, 1928, p.116). However, by 1896 it was routine, with 72 out of 84 surviving case notes showing patients received the test11). This evidence leads to the question of whether discourse does show change in cognition and calls for further analysis of practice and rhetoric at Bart's. The following detailed study of a Bart's physician may help to illuminate why discourse was so different from practice at St. Bartholomew's Hospital. [35]
The concept of "double lives" can be used as a device to try to understand why physicians' images were presented differently at different times, and why practice was different to language at Bart's. Samuel GEE is an ideal character to use as a case study as his representation in the secondary literature, and in the extracts of his own writings used within this, shows him to be apparently leading a completely different life to that shown by his medical practice on the wards at Bart's. [36]
Samuel GEE began his professional career at Bart's in 1870, becoming a full physician in 1878. He was Physician to the Prince of Wales from 1901. With his Headmasters' Conference school education at University College School, a London medical education, his interest in the history of medicine and a position in the royal household, GEE was a gentleman physician in LAWRENCE and PETERSON's definitions (BROWN, 1955, pp.183-4). [37]
GEE has been portrayed as an advocate of medicine as an art. Indeed, LAWRENCE (1998, p.96) quotes him as saying, "When you enter my wards your first duty is to forget all your physiology. Physiology is an experimental science—and a very good thing no doubt in its proper place. Medicine is not a science, but an empirical art"12). [38]
GEE "declined the honour of delivering the Harveian Oration at the Royal College of Physicians due to his disapproval of HARVEY's injunction to 'search and study out the secrets of nature by way of experiment'" (BODLEY SCOTT, 1974, p.185). As well as apparently being against laboratory science at the bedside (he was not opposed to physiology as a subject in its own right), he was quoted as being opposed to specialisation, proclaiming, "There is a name that I hate, yea there are two names that my soul abhoreth, the name of specialist and the name of a consultant" (BODLEY SCOTT, 1974, p.186)13). [39]
However, evidence from the clinical case notes from GEE's wards show that his patients received diagnostic assistance from the laboratory, therefore using experimental science performed by a specialist. Pathology had become specialised from 1893, when a full-time lecturer in pathology was appointed who lay the foundations of the Pathology Department during his four years at Bart's (WADDINGTON, 2003, p.117). GEE's patients were diagnosed with Widal's tests in six out of seven surviving typhoid records in 1899 (these are his earliest and only case files surviving after the discovery of the Widal's test). This shows an early and convincing acceptance of the worth of Widal's testing in cases of typhoid fever, which completely contradicts GEE's public image. For pulmonary tuberculosis and diphtheria, GEE's patients also increasingly received bacteriological laboratory tests from 1894-6. [40]
GEE's private notebooks show his use and opinions of bacteriology. These notebooks include notes from other authors, his own aphorisms, and also selected transcriptions of his case notes. In his extracts from case notes, it can also be seen that GEE (MS36, pp.135-6, 305 and 306) used the bacteriological laboratory for diagnosis of pulmonary tuberculosis between 1885 and 1891. [41]
GEE did not keep his use of the bacteriological laboratory secret. As well as carrying signs that GEE thought of medicine as an art, his Medical Lectures and Aphorisms, which went through at least four editions, includes the following examples of his use of bacteriology: GEE (1915a, p.74) included in an assessment of a case of chronic pituitous catarrh, read in front of the Royal College of Physicians, that "[t]ubercle Bacilli were not found." In discussing diagnosis of Bronchitis and Pulmonary Tuberculosis in the same lecture he mentioned the problems sometimes encountered using auscultation, but "since KOCH's discovery of the tubercle bacillus we have a potent auxiliary to diagnosis in the microscopic examination of the sputa" (GEE, 1915a, p.91). In his Aphorisms GEE (1915b, pp.244 and 266) said of cavernous bronchial breathing, that if it was caused by "tuberculous disease … discovery of tubercle bacilli would confirm it", and again concerning phthisis, that amongst all the methods of diagnosis, the most important was, "above all, detection of tubercle bacilli in the sputa". He even advised his medical students to tell patients suspected of being "phthisical" to "[s]ave your sputa to be tested (for bacilli)" (GEE, 1915b, p.246). Concerning typhoid accompanied by delirium, he considered that "testing the blood by cultivations of typhoid bacilli (Widal's test) must be employed as an additional means of diagnosis" (GEE, 1915b, pp.290-291). He also said, comparing himself with the empirical physician, in front of the Abernethian Society at Bart's in 1889, "I am ready to accept help from any source, from physiology and pharmacology, but also from mechanics, optics and similar sciences, from bacteriology, electricity and chemistry, nay very gratefully from cookery, upholstery, ironmongery, and indeed from any source" (GEE 1915c, p.238). [42]
He wrote a very similar comment privately, showing his conviction about the worth of other disciplines (GEE, MS34, pp.123-4). In discussing the process of the lungs becoming emphysematous, in a lecture to the Royal College of Physicians, he complained "unfortunately we can get no help from experimental pathology" in the same manner as it could be used for inflammation (GEE, 1915b, p.95). These public proclamations about the use of laboratory science in general show that GEE was not frightened to discuss its worth in front of eminent audiences. [43]
GEE's advocacy of opposing ideas was part of his personality. LEGG (1915, p.359) wrote that "GEE's character was exceedingly complex, and it is very difficult to unravel." GEE (1915c, pp.216 and 229; MS35, p.241) wrote publicly and privately about his dislike of dogmatism. In spite of these attacks on dogmatism, GEE (1915c, p.236) had a "kindly feeling" towards the "Empiric sect", which was, apparently, although in his category of dogmatic sects, "much less dogmatic" than his other examples. GEE is not the glowing example of an advocate of empiricism which he has been portrayed as though, as he states that "the empiric … is the ant which gathers facts but does not transmute them … his harvests are scanty. Well for him that all physicians are not empirics" (GEE, 1915c, pp.239-40)14). Indeed, LEGG (1915, p.363) considered GEE a sceptic15). GEE's lack of conviction about anything is demonstrated by LEGG's recollection that GEE's
"opinions on one subject, books or men, rarely last the same for any time. One would have talk with him, and a fortnight after resume the conversation at the point where it was left off and then it would be found that the whole tone of his thought had changed" (LEGG, 1915, p.380). [44]
Indeed, his aphoristic style of writing, privately, and publicly in HORDER's collection of his aphorisms, is perfect for GEE's undogmatic and eclectic way of thinking. GEE wrote privately, "[t]he advantage of the aphoristic way of writing is that no pretence of completeness is made; facts may be added without disarranging the structure" (GEE, MS34, p.124). GEE (MS34, pp.126 and 140-141) also doubted the reliability of new "facts", and wrote twice about this problem in his notebook. [45]
This doubt in GEE's thinking helps to explain why he may have been slightly reticent about the new experimental sciences infiltrating clinical medicine. He appears to have considered many innovations and new ideas, not accepting any belief in particular. He did not wholly accept empiricism or experimental science. LEGG's (1915, p.363) comment, "[t]hough he knew so much, yet his scepticism was very deep" sums up what is clear about GEE—he was interested in everything, accepted ideas and technologies on his own terms, and was ready to change his mind. [46]
Not surprisingly, GEE's discourse in his case notes was as complex as his writings and medical practice. In case notes supervised or written by him, "natural" and "normal" were used fairly equally in the 1880s and 1890s. However, use of "normal" for temperature far outweighed use for qualitative descriptions of organs and parts of the body. Therefore, GEE's notes are representative of patterns of use of language at Bart's in general. [47]
Recently, Lorraine DASTON and H. Otto SIBUM (2003) have discussed the possibility of scientists, and people in general, having different personae depending on the context. However, the traditional idea of double lives considers people have secrets to hide (GOFFMAN, 1969, especially Chapter 4). The case study of GEE questions this idea, showing that he did not hide his use of bacteriology. However, in this paper the use of the concept of "double lives" is a heuristic device in order to examine how gentlemen physicians were able to integrate the specialist laboratory into their clinical practice. The way in which GEE presented ways of using bacteriology to eminent audiences demonstrates that this was entirely possible. [48]
Part of the confusion regarding GEE's attitude towards experimental science may stem from his self-representation in the wards. In one of his notebooks, GEE (MS34, p.169) wrote:
"Always remember that the work in the Wards, so far as students are concerned, is simply the education of their senses. Pathology they can read at home. Waste no time over it. The pulse is dicrotous. What does dicrotism signify? Never mind, feel that it is dicrotous, + when you get home refer to your books." [49]
GEE may have given people the impression that laboratory science was not important to him by not "wasting time" discussing it on the wards. [50]
Gentlemen physicians may have presented various images of themselves in order to defend their profession. Diagnosis was perhaps the most important technique for a physician. Thomas HORDER and his colleague at Bart's, A.E. GOW (1952, p.xiii), considered diagnosis was the "be-all and the end-all" of medicine. Bacteriology was quite a threat to physicians, as their major role was being challenged (MAULITZ, 1979, p.92)16). There was reason for the physicians to be cautious about the impact of bacteriology, in order to defend their status. [51]
In the 1920s and '30s, HORDER (1937a, p.32; HORDER, 1937b, pp.174-5 and 181) seems to have been worried about the profession of the clinician due to the attitude of the public. In his experience, patients were growing increasingly convinced of the power of machines and experts. In 1924 he remarked on how lay people were treating doctors as though they had "no expert knowledge whatever", putting forward ideas such as possible causes of cancer (HORDER, 1924, p.822). Patients were coming to see him armed with X-rays and ideas about the reasons for their illnesses (HORDER, 1937b, p.183). He defended his profession, stressing the importance of "human judgment" (HORDER, 1937b, p.174). Patients were coming to him having already had diagnostic tests to save time and money. One patient would not allow HORDER to even examine him, saying, "please give me something for my headache: I don't want a diagnosis, it costs too much" (HORDER, 1937b, p.184). [52]
Professionally, however, the position of pathologist was not as grand as being a physician. Indeed, ANDREWES (1928, p.116) expected to become a physician at Bart's as he already held a position at the Royal Free Hospital. Giving this up was "a big change in one's life", but he realised he "loved laboratory work more than Out-Patients." The income of a pathologist was much lower than that of a hospital physician. Although the physicians had campaigned for £600 a year for the Bart's pathologist, he only received £100 with no time for private practice. The physicians were paid under 100 guineas at Bart's, but through private practice they could achieve huge salaries (SBH Ha 6/5 1895; SBH Ha 1/27 1895). The Bart's practitioners, Sir James PAGET and John ABERNETHY, from earlier in the nineteenth century, earned in excess of £10,000 a year at their peak (WADDINGTON, 1984, p.32). In a meeting between the Treasurer and the Medical Council at Bart's in 1895, the Treasurer said regarding the Medical Council's proposed salary for the Pathologist, "[o]f course £600 a year is not a large or even an adequate payment, but still all that class of work is not highly paid" (SBH Ha 6/5 1895). So, this low status of the bacteriologist shows why the physicians may have thought it safe to discuss the value of bacteriology in public. [53]
Case notes have been shown in this paper to have considerable worth in discovering what actually happened everyday in the life of the elite London hospital in the late nineteenth and early twentieth century. They reveal the change in rhetoric used in the hospital over time, and what this may have indicated for the "double life" of the physician—conflicted between the old world of bedside medicine and the new world of the laboratory, and holding onto the old world by continuing to use its language. [54]
Although Addenbrooke's Hospital was more similar to the U.S. in its reception of the laboratory, "natural" was still used more frequently at later dates than in the U.S. The difference in the domination of the term "normal" in Cambridge from the U.S. deserves further investigation, especially due to the prominence of experimental physiology in Cambridge. Differences between Bart's, and Addenbrooke's and the U.S., can be explained more easily. Older physicians had more of an influence on the creation of case notes at Bart's, the reputation of physiology teaching and research did not rival Cambridge, and the examination of GEE shows that medical practice was perhaps torn between an old and a new world for medicine, with physicians wanting to utilise the laboratory for the benefit of their practice, but perhaps afraid of the threat to their profession. It may also simply be that at Bart's there was a cognitive distinction between a quantifiable measure and a qualitative description meaning that though temperature was almost universally described as "normal", organs and features such as colour were not. This distinction can be further supported as the use of bacteriological methods was enthusiastically received so there was not an opposition to laboratory science. [55]
An examination of case notes based on language alone would represent Bart's as reluctant to accept the fruits of the experimental laboratory. So, at first glance, language does not mirror practice. However, using cluster analysis, especially of temperature, this is shown not to be the case, and perhaps this slight conservatism regarding language at Bart's relates to the confusing representations of the gentlemen physicians torn between a world based on bedside experience and one based on experimental science. [56]
I would like to thank the continued support of the Arts and Humanities Research Council, who have funded my career since embarking on my Masters degree in the History of Science, Medicine and Technology, including the doctoral thesis from which this paper has been developed. My PhD supervisor, Andrew MENDELSOHN has provided general wise advice for this paper, as have John Harley WARNER and Kati HANNKEN-ILLJES who both encouraged me to develop this work by conducting cluster analyses of the ways in which "natural" and "normal" were used. Thanks also to WARNER for kindly allowing me to reproduce the graph from The Therapeutic Perspective. The archivists at both St. Bartholomew's Hospital (Samantha FARHALL, Marion RAE and Katie ORMEROD) and Addenbrooke's Hospital (Hilary RITCHIE and Philip RUNDLE) have been very supportive, and have given me lots of useful advice on the history of the hospitals. Helpful assistance was also received in my research at the Royal College of Physicians, London. This work was originally prepared for the Kolloqium: "Diskurs, Zeit und Materialität", Freie Universität, Berlin, in 2004, and I would like to thank the members (especially Livia HOLDEN) of the Emmy-Noether Gruppe "Mikrosoziologie von Strafverfahren" for their invitation to present my work at this forum.
Addenbrooke's Hospital Archives, Cambridge
Medical casebooks, 1880-1920, AHPR1/1.
Royal College of Physicians, London
Samuel Gee, Volume III of Notes, 1865-, MS34.
Samuel Gee, Notebook I, 1873-. Notes re diseases, and case-notes, MS35.
Samuel Gee, Notebook V, 1879-. Notes re diseases, and case-notes, MS 36.
St. Bartholomew's Hospital Archives, London
Medical Registers, 1881-1920, MR 16.
Administration, Clerk's Office, Minutes of the Board of Governors, 11 May 1893 to 12 November 1903, Ha 1/27, House Committee, Thursday 14 March 1895.
Administration, Clerk's Office, Minute Book of Meetings of the Treasurer and Almoners and the Medical Council 1891-1902, Ha 6/5, Meeting, 17 January 1895.
Statistical Tables of the Patients under Treatment in the Wards of St. Bartholomew's Hospital, 1896.
1) The physicians of Bart's are particularly well represented in Christopher LAWRENCE's (1985) first article as advocates of character being highly important for the practice of medicine, including Patrick BLACK, Dyce DUCKWORTH and Sir James PAGET; a high prominence for Thomas HORDER in his second article on the subject, alongside Samuel GEE, Sir Percival HORTON-SMITH-HARLEY, and Sir Walter LANGDON BROWN (LAWRENCE, 1998); the 1999 article being entirely focused on the Bart's physicians GEE, HORDER, and BROWN (LAWRENCE, 1999); and the chapter of 2000 once again looking at GEE, HORDER, BROWN, the surgeon, D'Arcy POWER, and even William HARVEY, amongst other examples from the London and Oxford elites (LAWRENCE, 2000). In LAWRENCE's (1985, pp.516-17) first article on this topic, though, Thomas Lauder BRUNTON is portrayed as an advocate of diagnostic technologies such as the sphygmograph and sphygmomanometer, and fan of continental science, without mentioning he was a Bart's physician. Tensions between the laboratory and elite physicians in the clinic have also been examined for other countries (MAULITZ, 1979; GEISON, 1979; JACYNA, 1988). <back>
2) I use the word "specificity" with the opposite meaning to WARNER. He uses "specificity" and "universalism" to mean opposite ways of understanding disease. "Specificity" means "individualism" for him—the specificity of the patient—whereas in my research this term is used with reference to specific diseases (WARNER, 1997b). <back>
3) This sample of bacterial disease was chosen for wider research on the use of bacteriology in the Ph.D. thesis from which this paper is derived, "Using bacteriology in the hospital and in society: England, 1880-1939", Imperial College of Science, Technology and Medicine, University of London, forthcoming 2007. The case books listed amongst the references are not cited each time they are referred to in general as they are the main source for this paper. However, when Bart's case files or volumes are referred to individually they are separately cited in the manner SBH 16/number of case book/number of case note. Individual Addenbrooke's case notes are referenced AH box number/number of case book/number of case note. <back>
4) The hospital was opened in 1766, with the Regius Professor of Physic, Russell PLUMPTRE, as a physician to Addenbrooke's (ROOK et al., 1991, p.58). So there must only have been a small gap when the Regius Professor incumbent was not physician to the hospital. <back>
5) ROOK (1991, p.238) cites Sir W. LANGDON BROWN (1946). Some Chapters in Cambridge Medical History. Cambridge: Cambridge University Press. <back>
6) The professorship was not created at this time due to agricultural depression lowering Trinity College's income (GEISON, 1978, p.108). <back>
7) The vote was actually tied between ROY and the clinical pathologist, David James HAMILTON, but the Vice Chancellor of the University showed where his allegiance lay, voting for ROY (WEATHERALL, 2000, pp.139-140). <back>
8) WEATHERALL (2000, p.143) cites the Lancet (1884), 1, 911. <back>
9) Although this test is not very accurate, I have become very familiar with Samuel GEE's handwriting from looking through his private casebooks which are discussed later in this paper. I have not attempted this kind of analysis for any other physician as I do not have enough familiarity with their handwriting. <back>
10) WADDINGTON (2003, p.131) also presents bacteriology as being negatively received at Bart's in the 1880s and presents a picture of Samuel GEE being opposed to the use of the laboratory, so it is worth reconsidering his representation of the reception of experimental physiology at Bart's. <back>
11) The STATISTICAL REPORT (1896) shows that there were 92 cases of diphtheria admitted in 1896, so this is a very indicative sample. <back>
12) LAWRENCE (1998, p.96) cites Henry DALE (1950). Scientific Method in Medical Research. British Medical Journal, 2, 1187. <back>
13) See a similar comment in his private notebook (GEE, MS36, p.345). <back>
14) See LAWRENCE (2000, pp.47-49) for GEE being represented as "revering" empiricism. <back>
15) This is in GEE's opposing group to dogmatism (GEE, 1915c, p.242). <back>
16) LAWRENCE (1999, p.427) comments on diagnosis as the "cornerstone of medicine", repeated in LAWRENCE (2000, p.49). HAMMONDS (1999, p.11) also considers that change in diagnostic practices of diphtheria was seen as a threat to the medical profession of New York. <back>
Andrewes, Sir Frederick (1928). The beginnings of bacteriology at St. Bartholomew's. St. Bartholomew's Hospital Journal, 35(7/8), 100-104 and 116-117.
Bodley Scott, Ronald (1974). Medicine in the Twentieth Century. In Victor Cornelius Medvei & John L. Thornton (Eds.), The Royal Hospital of Saint Bartholomew 1123-1973 (pp.185-204). London: St. Bartholomew's Hospital.
Bourne, Geoffrey (1963). We met at Bart's: The autobiography of a physician. London: Friedrich Muller Limited.
Brown, G.H. (Compiler) (1955). Munk's roll, Volume IV: Lives of the fellows of the Royal College of Physicians of London, 1826-1925. London: Royal College of Physicians.
Cambridge Parliamentary and Municipal Borough (1927). Maps Fiche 2164(33), 25 inches: mile. Sheet XLVIII 2. British Library reference: Cambridgeshire Revised Edition, 47.2.
Cranefield, Paul F. (1957). The organic physics of 1847 and the biophysics of today. Journal of the History of Medicine and Allied Sciences, 12, 407-23.
Daston, Lorraine, & Sibum, H. Otto (2003). Introduction: scientific personae and their histories. Science in Context, 16, 1-8.
Elgaard Jensen, Torben (2007). Witnessing the future [59 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research [On-line Journal], 8(1), Art. 1. Available at: http://www.qualitative-research.net/fqs-texte/1-07/07-1-1-e.htm.
Ferris, Paul (1965). The doctors. London: Victor Gollancz Ltd.
Frank, Robert G. Jnr (1988). The Telltale Heart: Physiological instruments, graphic methods, and clinical hopes, 1854-1914. In William Coleman & Frederic L. Holmes (Eds.), The investigative enterprise: Experimental physiology in nineteenth-century medicine (pp.211-90). Berkeley, Los Angeles: University of California Press.
Gee, Samuel (1915a). On the causes and forms of bronchitis. Lecture given before the Royal College of Physicians (no date). In Samuel Gee, Medical lectures and aphorisms with recollections by J. Wickham Legg (pp.60-75). London: Henry Frowde, Oxford University Press and Hodder and Stoughton.
Gee, Samuel (1915b). Clinical aphorisms collected by Thomas Horder. In Samuel Gee, Medical lectures and aphorisms with recollections by J. Wickham Legg (pp.243-304). London: Henry Frowde, Oxford University Press and Hodder and Stoughton.
Gee, Samuel (1915c). Sects in medicine. Read before the Abernethian Society on June 20, 1889. In Samuel Gee, Medical lectures and aphorisms with recollections by J. Wickham Legg (pp.216-42). London: Henry Frowde, Oxford University Press and Hodder and Stoughton.
Geison, Gerald L. (1978). Michael Foster and the Cambridge School of Physiology: The scientific enterprise in late Victorian society. Princeton, New Jersey: Princeton University Press.
Geison, Gerald L. (1979). Divided we stand: Physiologists and clinicians in the American context. In Morris J. Vogel & Charles E. Rosenberg (Eds.), The therapeutic revolution: essays in the social history of American medicine (pp.67-90). Philadelphia: University of Philadelphia Press.
Goffman, Erving (1969). The presentation of self in everyday life. London: Allen Lane, The Penguin Press.
Hammonds, Evelynn Maxine (1999). Childhood's deadly scourge: The campaign to control diphtheria in New York City, 1880-1930. Baltimore: The Johns Hopkins University Press.
Horder, Thomas (1924). Individuality in medicine. An address delivered to the students of Durham University Medical College at the Opening of the Winter Session, Oct. 6th, 1924. The Lancet, ii, 819-24.
Horder, Thomas (1937a). The doctor as humanist. An address at the opening of the Westminster Hospital Medical School, 28th September 1936. In Thomas Horder, Health and a day: Addresses by Lord Horder (pp.19-41). London: J.M. Dent & Sons Ltd.
Horder, Thomas (1937b). The clinician's function in medicine. Read at the annual meeting of the Medical Society of the State of New York, 28th April 1936. In Thomas Horder, Health and a day: Addresses by Lord Horder (pp.164-184). London: J.M. Dent & Sons Ltd.
Horder, Thomas & Gow, Alexander E. (1952). The essentials of medical diagnosis: A manual for students and practitioners, revised with the assistance of Ronald Bodley Scott. London: Cassell and Company Ltd.
Howell, Joel D. (1987). "Machines" meanings: British and American use of medical technology, 1890-1930. Unpublished PhD thesis, University of Pennsylvania.
Jacyna, L.S. (1988). The laboratory and clinic: The impact of pathology on surgical diagnosis in the Glasgow Western Infirmary, 1875-1910. Bulletin of the History of Medicine, 62, 384-406.
Kontopodis, Michalis (2007). Fabrication of Times and Micro-Formation of Discourse at a Secondary School [88 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research [On-line Journal], 8(1), Art. 11. Available at: http://www.qualitative-research.net/fqs-texte/1-07/07-1-11-e.htm.
Lawrence, Christopher (1985). Incommunicable knowledge: Science, technology and the Clinical Art in Britain, 1850-1914. Journal of Contemporary History, 20, 503-520.
Lawrence, Christopher (1998). Still incommunicable: Clinical holists and medical knowledge in interwar Britain. In Christopher Lawrence & George Weisz (Eds.), Greater than the parts: Holism in biomedicine, 1920-1950 (pp.94-111). New York: Oxford University Press.
Lawrence, Christopher (1999). A tale of two sciences: bedside and bench in Twentieth-Century Britain. Medical History, 43, 421-449.
Lawrence, Christopher (2000). Edward Jenner's jockey boots and the great tradition in English medicine 1918-1939. In Christopher Lawrence & Anna-K. Mayer (Eds.), Regenerating England: Science, medicine and culture in inter-war Britain (pp.45-65). Amsterdam: Rodopi.
Legg, J. Wickham (1915). Recollections of Samuel Gee, physician to Saint Bartholomew's Hospital brought together by J. Wickham Legg. In Samuel Gee (Ed.), Medical lectures and aphorisms with recollections by J. Wickham Legg (pp.353-392). London: Henry Frowde, Oxford University Press and Hodder and Stoughton.
Maulitz, Russell C (1979). "Physician versus bacteriologist": The ideology of science in Clinical Medicine. In Morris J. Vogel & Charles E. Rosenberg (Eds.), The therapeutic revolution: Essays in the social history of American medicine (pp.91-107). Philadelphia: University of Philadelphia Press.
Moreira, Tiago (2007). How to investigate the temporalities of health [60 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research [On-line Journal], 8(1), Art. 13. Available at: http://www.qualitative-research.net/fqs-texte/1-07/07-1-13-e.htm.
Motzkau, Johanna F. (2007). Matters of suggestibility, memory and time: Child witnesses in court and what really happened [42 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research [On-line Journal], 8(1), Art. 14. Available at: http://www.qualitative-research.net/fqs-texte/1-07/07-1-14-e.htm.
Peterson, M. Jeanne (1978). The medical profession in Mid-Victorian London. Berkeley, Los Angeles: University of California Press.
Porter, Roy (2001). Bodies politic: Disease and death and doctors in Britain, 1650-1900. Ithaca, New York: Cornell University Press.
Rook, Arthur; Margaret Carlton & Cannon, W. Graham (1991). The history of Addenbrooke's Hospital, Cambridge. Cambridge: Cambridge University Press.
Waddington, Ivan (1984). The medical profession in the Industrial Revolution. Dublin: Gill and Macmillan Ltd.
Waddington, Keir (2003). Medical education at St. Bartholomew's Hospital 1123-1995. Woodbridge, Suffolk: The Boydell Press.
Warner, John Harley (1997a). The therapeutic perspective: Medical practice, knowledge, and identity in America, 1820-1885. Princeton, New Jersey: Princeton University Press.
Warner, John Harley (1997b). From specificity to universalism in medical therapeutics: Transformation in the 19th-Century United States. In Judith Walzer Leavitt & Ronald L. Numbers (Eds.), Sickness and health in America: Readings in the history of medicine and public health (pp.87-101). Madison, Wisconsin: University of Wisconsin Press.
Weatherall, Mark W. (2000). Gentlemen, scientists and doctors: Medicine at Cambridge, 1880-1940. Woodbridge, Rochester, New York: Boydell Press in association with Cambridge University Library.
White Franklin, Alfred (1974). Medicine in the eighteenth and nineteenth centuries. In Victor Cornelius Medvei & John L. Thornton (Eds.), The Royal Hospital of Saint Bartholomew 1123-1973 (pp.126-184). London: St. Bartholomew's Hospital.
Worboys, Michael (2004). Private clinical laboratories in Britain: The Clinical Research Association, 1894-1914. Unpublished paper presented at the American Association for the History of Medicine Annual Conference, Madison, Wisconsin.
Rosemary WALL undertook this research for part of a chapter in the forthcoming doctoral thesis, "Using bacteriology in the hospital and in society: England, 1880-1939", Centre for the History of Science, Technology and Medicine at Imperial College of Science, Technology and Medicine, University of London from 2003-2006. From October 2006 she began a two-year AHRC post-doctoral research position at the Wellcome Unit for the History of Medicine, University of Oxford, researching the history of medicine in late colonial Kenya, building on research already completed for her MSc dissertation at Imperial College.
Contact:
Rosemary Wall
Wellcome Unit for the History of Medicine
45-47 Banbury Road
Oxford
OX2 6PE, UK
E-mail: rosemary.wall@wuhmo.ox.ac.uk
Wall, Rosemary (2007, January). "Natural", "Normal": Discourse and Practice at St. Bartholomew's Hospital, London, and Addenbrooke's Hospital, Cambridge, 1880-1920 [56 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 8(1), Art. 17, http://nbn-resolving.de/urn:nbn:de:0114-fqs0701174.