

Volume 20, No. 3, Art. 13 – September 2019
Mastering Treatment for Sleep Apnoea: The Grounded Theory of Bargaining and Balancing Life With Continuous Positive Airway Pressure (CPAP), in the Context of Decisional Conflict and Change Theories
Kim Ward, Merryn Gott & Karen Hoare
Abstract: Continuous positive airway pressure (CPAP) treatment for sleep apnoea can be challenging for patients to master. Given limited evidence on this topic, we used constructionist grounded theory methodology to explore experiences of living with CPAP from participants' perspectives. Adults (n=16) were recruited through a main-center respiratory service in New Zealand and participated in semi-structured interviews. Data were analyzed until theoretical saturation was achieved.
In this article, we present the newly constructed grounded theory of bargaining and balancing life with CPAP, which explains how participants made a series of personal decisions about whether to use and how to master CPAP. To situate, support and provide explanatory power the new theory is discussed in the context of change and decision theories to illustrate the varying phases of readiness experienced by persons preparing to engage with CPAP and the decision-making process required for effective management of CPAP at home.
This study provides valuable CPAP-user centered information for the development of interventions to optimize CPAP use. Acknowledging individuals' abilities to make reasoned healthcare decisions and providing clinical environments that support the active process of bargaining and balancing may increase uptake of CPAP, and potentially other long-term therapies.
Key words: chronic illness; continuous positive airway pressure; grounded theory methodology; patient perspectives; sleep apnoea; storyline
Table of Contents
1. Introduction
2. Methods
3. Findings: Bargaining and Balancing Life With CPAP
4. Discussion
4.1 Bargaining and balancing and change theory
4.2 Bargaining and balancing and decision theories
4.2.1 Rational choice theory underpinning bargaining and balancing life with CPAP
4.2.2 Decisional conflict theory underpinning bargaining and balancing life with CPAP
5. Conclusion
Globally, sleep-disordered breathing represents an increasingly significant component of clinical respiratory care management, exceeded only by asthma and chronic obstructive pulmonary disease (BARBÉ & PÉPIN, 2015; McNICHOLAS & BONSIGNORE, 2010). Obstructive sleep apnoea (OSA) is the most common sleep-related breathing disorder, affecting millions of people worldwide (BARBÉ & PÉPIN, 2015). OSA describes the presence of intermittent partial or complete obstruction of the pharynx that is associated with snoring, sleep fragmentation, daytime sleepiness and related consequences. Typically, people with OSA are overweight, older men. However, sufferers also include women, younger men, and lean individuals with altered maxillofacial architecture (BARBÉ & PÉPIN, 2015; MAY et al., 2018). With the advent of improved diagnostics, the prevalence of OSA has become evident, as has the impact on health and the socioeconomic burden of untreated OSA (HILLMAN, MURPHY & PEZZULLO, 2006). [1]
The most common treatment for sleep apnoea is overnight continuous positive airway pressure (CPAP) delivered via a full face or a nasal mask connected to a bedside CPAP machine. The device delivers air under pressure that pneumatically splints the upper airway during sleep. Considered the gold standard therapy for sleep apnoea, CPAP has been recognized as a cost-effective treatment for OSA since the early 1980s (GILES et al., 2008; QASEEM et al., 2013; SULLIVAN, BERTHON-JONES, ISSA & EVES, 1981). A significant body of research conducted since the 1980s has improved the function of the CPAP device and mask and has increased understanding of the consequences of untreated sleep apnoea. Nevertheless, concern exists that CPAP is under-utilized by sleep apnoea sufferers and that poor compliance jeopardizes clinical outcomes (GHOSH, ALLGAR & ELLIOTT, 2013; GORDON, WU, MUNNS, DeVRIES & POWER, 2018; MCEVOY et al., 2016; VAN ZELLER, SEVERO, SANTOS & DRUMMOND, 2013; WOHLGEMUTH, CHIRINOS, DOMINGO & WALLACE, 2014). CPAP can be challenging for patients; mask fitting can be difficult as can accommodating to lifelong CPAP therapy. Accordingly, most information available about using CPAP derives from research that explores interventions to improve compliance (MAY et al., 2018; MORAN HIGHSMITH, LEHOCKEY & EVERHART, 2012; SAWYER et al., 2011; SMITH, LASSERSON & HANIFFA, 2004; WOZNIAK, LASSERSON & SMITH, 2014) [2]
Although non-compliance with CPAP is a concern, only partial clarity exists around issues that may influence peoples' CPAP use (WARD, HOARE & GOTT, 2014). While consideration of the difficulties experienced by patients is evident in the literature, interest in the patients' views about their experience has been limited to date. To address this gap in knowledge, we chose grounded theory methodology (GTM) to explore living with CPAP and construct a theory that explains how patients live with this treatment in daily life (CHARMAZ, 2014). It is important in GTM to consider relevant extant theories to situate, support and provide explanatory power to a new grounded theory (BIRKS & MILLS, 2015; CHARMAZ, 2014). Therefore, in this article we present the new grounded theory and situate findings in the context of change and decision theory. Applying the grounded theory in sleep medicine and other long-term care environments may contribute to an understanding of how patients view their therapies. Such insights may promote increased uptake of long-term treatment such as CPAP by supporting decision-making processes and can prove useful for fostering good use of therapy. [3]
We begin by outlining the methods used to generate and analyze the data (Section 2). In Section 3, using storyline technique, we present findings that support the new substantive theory of bargaining and balancing life with CPAP. Thereafter, we discuss the significance of findings from the study by aligning them with existing theories relevant to bargaining and balancing life with CPAP (Section 4), followed with a concluding section (Section 5). [4]
We employed a qualitative design using constructionist grounded theory methodology (CHARMAZ, 2014). Data were generated from individual in-depth, semi-structured interviews, to garner rich and detailed information (KVALE & BRINKMANN, 2009). National and local ethics committees gave ethics approval (reference NTX/11/06/048/AMO2). Adult participants were recruited from a major city respiratory clinic in New Zealand (n=16). Initial participant sampling was purposive with a focus on recruiting adults with personal knowledge of using CPAP. Additional participants were sampled theoretically based on information they might provide (BIRKS & MILLS, 2015; CHARMAZ, 2014). In total, sixteen participants were recruited (women n=7, men n=9). People aged seventeen years and under, or those prescribed CPAP for other illnesses were excluded. [5]
KW conducted, audio-recorded, transcribed and coded all interviews over ten months ending in late 2014. The average interview duration was 52 minutes, the shortest being 24 minutes and the longest 82 minutes. Interview data and interview notes were stored and managed using QSR NVivo10. Interviews began with open-ended questions or prompts to elicit information relevant to the participant regarding CPAP. These included: "Tell me about your CPAP, and about your night-time routine?"; "What does CPAP mean to you?"; and "How do you explain sleep apnoea or CPAP to others?" KW followed new avenues of inquiry as new categories were constructed from the data (BIRKS & MILLS, 2015; KVALE & BRINKMANN, 2009). Subsequent questions focused on exploring and developing main categories. [6]
Data were analyzed using a grounded theory approach with the coding framework inductively derived from the data (WARD, HOARE & GOTT, 2017a). Since data collection and analysis occur concurrently in GTM, analysis commenced with line-by-line coding of the first transcript to identify initial constructs (BIRKS & MILLS, 2015; CHARMAZ, 2014). Lower-level categories were clustered into main categories, followed by integration into the final theory. As analysis progressed, the constant comparative process enabled adaptation and development of increasingly focused questions to explore new ideas and facilitate saturation of the main categories. Memoing and diagramming bolstered theory integration and data collection concluded once theoretical saturation of categories had occurred (CHARMAZ, 2014). [7]
3. Findings: Bargaining and Balancing Life With CPAP
Bargaining and balancing life with CPAP revolves around the wish for a good sleep and explains how participants grew accustomed to using CPAP to improve sleep. Bargaining and balancing explains the process of decision-making that participants engaged in to change their daily routines and begin lifelong CPAP use. The theory comprises three main categories, becoming a team for good-sleep, making choices about CPAP and becoming used to CPAP. This theory operated in the minds of the participants as they bargained and balanced both in debate with themselves about using CPAP and in relationships with those around them as they solved problems and reached decisions about using CPAP together. In Figure 1, we depict the theory's main categories and sub-categories.
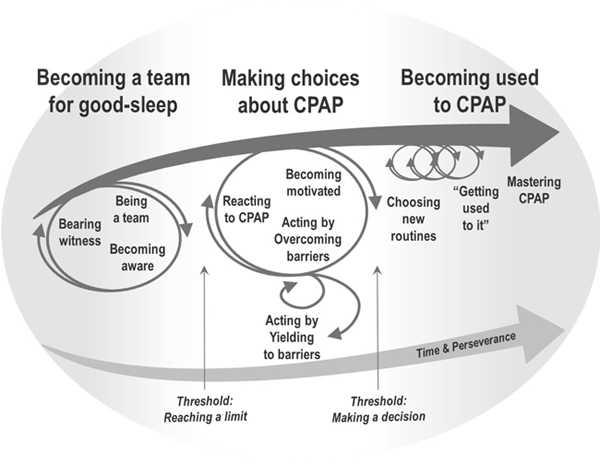
Figure 1: Model of the theory: Bargaining and balancing life with CPAP [8]
The top arrow in Figure 1, pointing left to right, illustrates a pathway of decision-making with a beginning, middle and end. Participants progressed in one direction through the three phases of the pathway, starting with becoming a team for good-sleep. The circular arrows in Figure 1 represent periods in which participants bargained and balanced the advantages and disadvantages of using CPAP. The size of the circular arrows in Figure 1 portrays the iterative nature and intensity of negotiation. For example, in the first category, there were significant negotiations between partner and spouse to have the person snoring understand what a problem it was. By the third category, partners continued to encourage the snorer to use CPAP so all concerned could sleep well, but personal bargaining and relational negotiation were far less intense, shown by the smaller circular arrows in Figure 1. [9]
Using an extended storyline technique, the following details the theory of bargaining and balancing life with CPAP (BIRKS, MILLS, FRANCIS & CHAPMAN, 2009; STRAUSS & CORBIN, 1990). Data that evidence detailed elements of main categories are reported elsewhere so are focused on the overall theory here (WARD, HOARE & GOTT, 2017b, 2018). Sub-categories and each of the main categories are italicized. [10]
Becoming a team for good-sleep, the first main category, explains the role of partners in bargaining and balancing life with CPAP. Partners catalyzed the process of becoming aware by bearing witness to the effect of sleep apnoea on loved ones. Partners enacted bargaining with loved ones to seek help so that both parties could sleep well. Consequently, snorers and partners began being a team who collaborated with initiating and integrating CPAP into daily life. [11]
This category began with partners, and occasionally family or friends, bearing witness to OSA symptoms that lead to poor sleep for both witnesses and snorers. Witnesses drew snorers' attention to how often they fell asleep during social occasions or caused concern for them while asleep. Participant (P) 13's grandchildren told her, "Nana, we can hear you [snoring] from up the road!" and P5 stated: "My partner [would] wake me up regular times during the night thinking I might die because I'd stopped breathing." [12]
The impact of any given symptom differed for each participant. However, it required bargaining by witnesses, together with an awareness of symptoms, to prompt the snorer to seek treatment. P9 described negotiating with his partner to seek help: "In the end, I kinda harassed him enough that he went to the doctors. He'd obviously get quite annoyed about it, 'cause he wasn't really aware how bad it [snoring] was." [13]
Witness' testimony enabled snorers to start becoming aware of symptoms, such as apnoeic episodes and snoring, and initiated a collaborative team process with the aim of improved sleep for both parties. Participants began being a team focused on initiating and integrating CPAP. Partners also spoke of balancing their need for a good sleep against allowing their loved one to retain personal responsibility for CPAP use. Reports of the challenging nature of balancing needs and negotiating reciprocal sleep captured the difficulties of bargaining in relationship during this preliminary category: "It's quite hard, 'cause I don't wanna come across as like, 'did you remember, did you remember!' ... But I try not to because it's not really my equipment and my responsibility" (P9). [14]
This comment illustrated the on-going negotiation required during interactions between partners and CPAP-users. Successful negotiation catalyzed the decision to act and improve sleep by seeking medical help and facilitated joint therapy management with the promise of good sleep. [15]
The second category, making choices about CPAP, describes how, on receiving a CPAP device, participants balanced the positives and negatives of CPAP use and bargained with themselves to make a definitive decision about using CPAP. This category comprises the subcategories reacting to CPAP, becoming motivated, and acting by overcoming barriers or by yielding to barriers. Participants began with reacting to needing CPAP in which they reported disappointment about receiving the device or described being embarrassed or ashamed about wearing the mask and fearing what others would think. P4 described the mask as "Darth Vader" like and P2 referred to the "stigma of the thing" and felt being single protected him from "disparaging comments" by others. Moreover, participants described a perception that mainly overweight older men suffered OSA. This perception dismayed CPAP-users who described themselves as young, fit or female. P12 remarked, "how could that be me?" Several participants sought ways to assure the need for CPAP before engaging with it. Indeed, P5 had three different surgeries to treat his sleep apnoea along with weight loss and concluded, "that the only opportunity now is the machine." More commonly, participants reported relief at finally having a solution to snoring and sleepiness and that symptoms were not "just imagined" (P6). Consequently, they devised various strategies for becoming motivated to use the device, the second sub-category. Comparing and balancing how unwell they felt before CPAP with subsequently enhanced wellbeing affirmed the positive consequences of CPAP and supported prioritizing CPAP:
"I wish I didn't have to put it on ... but the payoff, feeling OK when you wake up ... it doesn't really make it too questionable. I actually look forward to getting in bed and sticking it on, despite my embarrassment, because of my renewed energy levels" (P5). [16]
Feeling well was a tangible experience and made the balance of reasons to use CPAP fall in favor of continued use. Most participants described CPAP as "good for" them and as "a solution" that worked as promised because snoring stopped, they felt well and their partners were "really happy." Therefore, balancing the positive consequences of CPAP against perceived negatives supported the motivation to prioritize CPAP. [17]
Participants who did not immediately feel well balanced the promised but intangible returns of using CPAP against the challenges they encountered. P12 said the mask was "hideous, but you feel more hideous if you don't use it." Each participant identified the gravity of his or her diagnosis and balanced the physiological consequences of untreated sleep apnoea against the risk posed to cardiovascular health. Likewise, participants feared the life-limiting nature of untreated sleep apnoea and described how improved oxygenation during sleep would increase physical and psychological well-being. P11 was firm in her view that without CPAP her husband "would be dead." Consequently, balancing the risk of poor health against the promise of "long life" also became motivating (P7). Additionally, participants reported various struggles with CPAP and that becoming motivated facilitated overcoming barriers, the third sub-category. Struggling with the mask was common and users engaged in the process of "trial and error" to deal with discomfort (P8). [18]
Bargaining and balancing also led to choosing another way to manage sleep apnoea rather than use CPAP by yielding to barriers, the fourth subcategory. While one participant eventually chose to avoid CPAP use, for most the process of overcoming and yielding to barriers was cyclical as participants yielded to barriers intermittently, reasoning that they could get away without CPAP at any given moment. P1 recounted occasionally reaching a point during the night of having worn CPAP for "long enough" and removing the mask to have a "proper sleep." He stated that using CPAP protected his health, meant he slept well and woke "refreshed." However, it was only sleeping without the mask that was "proper." The contradiction in his comments spoke to how participants swung between fully endorsing CPAP use and "getting away" without it and that this could happen in the moment as well as over time. This swing reflected participants' inner battle to balance personal pros and cons of CPAP use. [19]
Through bargaining and balancing, personally and with their partner, CPAP-users processed reactions to needing CPAP and developed motivations regarding CPAP use, which for most led to the start of becoming used to CPAP, the final category. Participants who remained motivated and persevered with the choice to use CPAP began creating a "business as usual" scenario (P9). This category begins with choosing new routines, which together with the second subcategory getting used to it, resulted in mastering CPAP. [20]
Participants made adaptations to established routines and rituals to cement the intention to become used to CPAP by choosing new routines and adapting "just the little things" that enabled "re-learning" of night-time routines to accommodate CPAP (P5). CPAP-users and partners collaborated to negotiate new routines, such as when to turn out the light or fit sex around using CPAP: "I suppose, in the bedroom sexual wise ... you can't be quite so spontaneous, but that's fine too, we're not as young as we used to be" (P14). [21]
Once the challenges of using CPAP had receded, making CPAP a normal part of life was relatively straightforward and with time "just became the routine" (P4, P7, P12 and P15). CPAP-users and partners now had the same goal, "which is that he sleeps properly, and therefore, I sleep properly" (P8). Subsequently, negotiation between partners became a less intense maintenance process of gentle reminders to use CPAP, rather than the more intense bargaining in the first category that brought snorers to awareness of sleep apnoea:
"... if I go up to bed first, and I fall asleep before I've put my mask on ... I'll be aware of Baby standing there going 'mum, mum, put your mask on, you're making terrible noises'. It's just a normal thing in our family now" (P12). [22]
While establishing routines, participants described "getting used to" using CPAP. Each participant used the phrase "getting used to it" in varying contexts, making this a fitting in-vivo code that was elevated to the second subcategory. For some, becoming accustomed to CPAP was quick and unproblematic, while others required time and effort troubleshooting the device and mask, explaining "it took a bit to get used to it" (P5). Participants used the phrase "getting used to it" in different tenses depending on their stage of CPAP use. Those in the first months of treatment expressed an expectation they would get used to it and made a conscious decision to do so. Others spoke of having trouble, but expecting that eventually, they would become accustomed to it. Participants also described needing to get used to it, being in the process of or already being used to it:
"I hated it when I first had it. The first few nights I ripped it off and threw it across the room. I said to my partner it's like having a Hoover on backwards and someone's shoved the hose in your mouth. But, you know, I'm used to it now" (P4). [23]
By reinforcing and embedding the change into everyday life, and in the presence of time and perseverance, mastering CPAP became possible. P15 captured the relationship between persevering, the passage of time and getting used to CPAP: "Persevere for a while, and then you'll get used to it and then you won't ever want to be without it." [24]
Participants continued to bargain and balance in a small way until using CPAP was no longer in question. Participants frequently used the word just to signify that using CPAP no longer required conscious effort, and other matters occupied participants' thoughts. P13 concluded, "of course, you just put it on each night and you hardly even notice." Becoming used to CPAP by transforming new routines into everyday activities rendered CPAP mundane as it receded into the minutiae of daily life. Nevertheless, CPAP remained undiminished in its importance in maintaining good sleep for users, their partners and other family members. [25]
This article is the first to present a constructed grounded theory that explains users' perspectives of using CPAP through bargaining and balancing personally and in close relationship with others. In this article, we advance knowledge by identifying the CPAP-users as active, reasoned decision-makers in their healthcare, and without focusing on adherence. Data drawn from this study support the concept of a process of bargaining and balancing to manage decisions and change associated with using CPAP. Motivated decision-making by participants sustained those who had challenges getting used to CPAP and supported others' pragmatic decision to "just get on with" using CPAP. Participants made reasoned decisions based on reactions to CPAP, beliefs about pertinent motivating factors and the information available. Our findings have resonance with similar studies in chronic kidney disease and cancer management that illustrate how the decision-making process corresponds with personal views about treatment and personal life (FASSE et al., 2017; HARWOOD & CLARK, 2013; JOHANSSON, 2013; TONG et al., 2013). Indeed, we argue that change and decision theories may underpin the strategies of bargaining and balancing for patients using CPAP and other long-term treatment. [26]
To provide a platform for a discussion about the significance of findings from this study, we align existing theories relevant to bargaining and balancing life with CPAP. It is important in GTM to explore relevant extant theories to situate and validate a new grounded theory (CHARMAZ, 2014). Relevant extant theories give explanatory power and increase the potential for applicability beyond the substantive area of research (BIRKS & MILLS, 2015). Moreover, by using existing theories, the discussion that follows draws this grounded theory into wider debate. Since no single extant theory supports the complete bargaining and balancing process engaged in by participants, we integrate theories that support separate elements of the process. [27]
4.1 Bargaining and balancing and change theory
Through bargaining and balancing participants identified themselves as reasoned decision-makers in their healthcare and more than capable of making a change in their lives to use CPAP (WARD et al., 2017b). Behavioral scientists have extensively explored health-related decision-making processes, resulting in the development of various behavior change theories (CLARK & JANEVIC, 2014). The trans-theoretical model of change offers an integrative framework incorporating central constructs that include stages of change and decisional balance (PROCHASKA, 2013; PROCHASKA & DiCLEMENTE, 1983). The stage of change construct corresponds to different phases of readiness experienced by persons preparing to engage in a new behavior (MARCUS, EATON, ROSSI & HARLOW, 1994). PROCHASKA and DiCLEMENTE (1983) identified five distinct phases of change: pre-contemplation or not intending to change; contemplating a change; preparing to change; acting by engaging in the new behavior, and maintaining the change over time. Accordingly, sleep medicine researchers have used the trans-theoretical model to explain poor CPAP adherence (SAWYER et al., 2011; STEPNOWSKY, MARLER & ANCOLI-ISRAEL, 2002; WEAVER et al., 2003; WILD, ENGLEMAN, DOUGLAS & ESPIE, 2004). Research teams led by ALOIA and STEPNOWSKY used elements of the model to clarify inconsistencies in determining reasons for poor adherence to CPAP (ALOIA, ARNEDT, STEPNOWSKY, HECHT & BORRELLI, 2005; ALOIA, ARNEDT, STRAND, MILLMAN & BORRELLI, 2013; STEPNOWSKY, MARLER, PALAU & BROOKS, 2006; STEPNOWSKY, BARDWELL, MOORE, ANCOLI-ISRAEL & DIMSDALE, 2002). However, application of the trans-theoretical model to compliance with CPAP has proven inconclusive, with only ALOIA et al. (2005) finding elements of the model predictive of adherence to CPAP at six months after treatment initiation (MORAN et al., 2012). [28]
Data from this study reflect the last four stages of change, as participants had already initiated the change to using CPAP. Nevertheless, moving from engaging in the new behavior to maintaining the change over time oversimplifies the to-and-fro process of engaging and disengaging in CPAP use that participants experienced while making choices to use CPAP. Therefore, application of the trans-theoretical model overlooks how participants internally debated and oscillated between decisions before settling on one. The model also proposes that people who identify more pros than cons to using a treatment, such as CPAP, will become accustomed to it (PROCHASKA, 2013). Indeed, those participants who devised personal motivations to use CPAP, such as noticing that they felt better when they used it, were likely to have progressed to mastering CPAP. Based on our data, we argue that progress through phases is more dynamic than linear and occurs at varying rates, as evidenced by the time-based qualities of the subcategory, getting used to CPAP. For example, some participants remained caught in contemplation and preparation, expecting that eventually, they would get used to CPAP, while others moved quickly to the maintenance and mastery stages of CPAP use, having "got used to it." The decisional balance construct of the trans-theoretical model, underpinned by decision theory, more clearly explains this fluid decision-making process. [29]
4.2 Bargaining and balancing and decision theories
Reaching a decision by making choices among given alternatives requires a series of continuous cognitive processes. RAPOPORT (1998) identifies that decision theory attempts to describe and predict these cognitive processes by assuming that a decision has consequences and that actors prefer a particular consequence. Decision theory in its broadest sense describes societal processes that bring about group decisions, known as game theory or social process theory. Decision theories reflect the inclination to select a choice that is optimal when compared to personal preferences and beliefs, and to any constraints encountered. Normative decision theory focuses on predicting decisions by "perfectly rational" actors to identify how individuals or groups would or ought to behave in a given choice situation (KTE'PI, 2013; RAPOPORT, 1998; SLOVIC, FISCHHOFF & LICHTENSTEIN, 1977). However, decision theories also deal with aspects of selecting a choice from a range of possibilities by an individual (KTE'PI, 2013). These are descriptive decision theories that are primarily inductive and emphasize that a person's decision is optimal from specifically his or her point of view (RAPOPORT, 1998). Therefore, descriptive decision theories focus on making sense of how people make decisions, which aligned with the focus of this study on how people live with CPAP. Two such theories include rational choice theory and JANIS and MANN's (1977) conflict theory model of decision-making. [30]
4.2.1 Rational choice theory underpinning bargaining and balancing life with CPAP
Originally developed as a theory of decision-making in economics, sociologists developed a focus on rational choices made by individuals as studies produced evidence to support the relevance of the theory in areas such as family, religion and gender (BRAHAM, 2013; BRÜDERL & KALTER, 2001; DIJKSTRA, LINDENBERG & VEENSTRA, 2007; KRONEBERG & KALTER, 2012; OPP, 1999). In departing from its economic basis, sociologists adapted and modified the core assumptions of rational choice theory to include the premises that personal beliefs and constraints can be both objectively and subjectively perceived; that the desire to act aligns with personal identity, values and internalized norms; and that preferences can encompass a diversity of motivations such as altruism or fairness (KRONEBERG & KALTER, 2012). These premises correspond closely with participants' experiences. For example, participants' personal beliefs and knowledge about sleep apnoea and CPAP did not always correspond with empirical evidence; one participant determined that losing weight was the answer to treating his sleep apnoea, and others had believed sleep apnoea was limited to overweight older men. Objective constraints included problems with mask-fitting, and subjectively perceived constraints such as other peoples' potential negative thoughts about CPAP. Others were motivated to use CPAP by a desire to be fair to partners and facilitate their sleep rather than for personal health and welfare. [31]
Rational choice theory assumes that striving to optimize balance between goals or preferences in the presence of restrictions results in choices that determine behavior (BRAHAM, 2013; SCOTT, 2000). For instance, participants assessed the pros and cons of using CPAP and balanced these against the actual or anticipated benefits of using CPAP such as the preference to sleep well, whether this was with or without CPAP. BOUDON (2003) highlights that rational choice theory describes choices that are subjectively rational from the chooser's point of view (RAPOPORT, 1998). Thus, someone might opt to abandon CPAP despite understanding the risks and consequences of untreated OSA, or might decide to persevere with CPAP despite significant mask-fitting difficulty. Although a variety of factors described by participants align with the assumptions of rational choice, critics claim that it ignores the impact of an impulsive, emotional, altruistic or habitual action (BRAHAM, 2013). Indeed, GOLDTHORPE (1996) argued that rational choice assumes people make decisions with full knowledge and without being conflicted. Therefore, while rational choice theory corresponds to part of the processes described during the second main category of this study, it does not explain how all participants made choices between conflicting priorities, such as balancing the impulse to remove an uncomfortable mask against the knowledge that keeping it on would improve their health. [32]
4.2.2 Decisional conflict theory underpinning bargaining and balancing life with CPAP
Data drawn from the second main category reflects decision-making in the context of conflicting motivations that cause cognitive dissonance. JANIS and MANN's (1977) decisional conflict model, which states people avoid information that conflicts with their beliefs, provides added explanatory power to bargaining and balancing. JANIS and MANN proposed that individuals behave according to five coping patterns when faced with a choice regarding a course of action (JANIS, 1985; JANIS & MANN, 1976, 1977). Typically, threat-based stress, such as an emergency warning or a message that urges protective action, precipitates the need to choose a course of action (JANIS & MANN, 1976). In this context, a sleep apnoea diagnosis represents a threat-based message with implications for heart health and longevity, as reflected by P8's comment: "You read about how much [sleep apnoea] affects you, and heart disease and all that. That's my concern; long term effects that can have a drastic effect on your lifespan." [33]
The decision to use CPAP is, therefore, a protective one. The coping patterns that comprise decisional conflict theory are un-conflicted inertia, un-conflicted change, defensive avoidance, hyper-vigilance and vigilance. The vigilance coping pattern describes an adaptive process that leads to high-quality decisions which, in this case, would mean using CPAP. The other four coping patterns can be adaptive but are more often described as resulting in poor decision-making with poor consequences (BOUCKENOOGHE, VANDERHEYDEN, MESTDAGH & VAN LAETHEM, 2007; JANIS, 1985). In Table 1, we outline the five coping patterns.
|
Coping pattern |
Description of pattern |
Loss from not changing |
Loss from changing |
|
Un-conflicted inertia |
Decision ignored, status quo is maintained. Interest in information about the issue is low. |
Low |
High or low |
|
Un-conflicted change |
Decision to change made without question. Interest in information about the issue is low. |
High |
Low |
|
Defensive avoidance |
When there is no hope of finding a better solution procrastinating, shifting responsibility or wishful thinking occur. Exposure to information is selective and affirms the decision maker's choice. |
High |
High |
|
Hyper-vigilance (or "panic") |
When there is not time or hope of finding a better solution information gathering is hurried and poorly evaluated leading to hasty decisions that seem to promise immediate relief but overlook the full range of consequences. |
High |
Low or high |
|
Vigilance |
When there is time and hope of finding a better solution information gathering, assessment and evaluation of options are considered and balanced before making a decision. |
High |
Low or high |
Table 1: Coping patterns of JANIS and MANN's decisional conflict theory [34]
Regarding un-conflicted inertia, interest in information about symptoms had led participants to seek medical help. Therefore, they had decided to start using CPAP, rather than ignore the need for treatment altogether. A criterion for hyper-vigilance is a lack of time. However, all participants reported having had time to think about using CPAP. Data drawn from this study corresponds to the other described coping patterns. In Figure 2, we provide a graphic representation based on JANIS and MANN's model to illustrate participants' coping styles during the decision-making process.
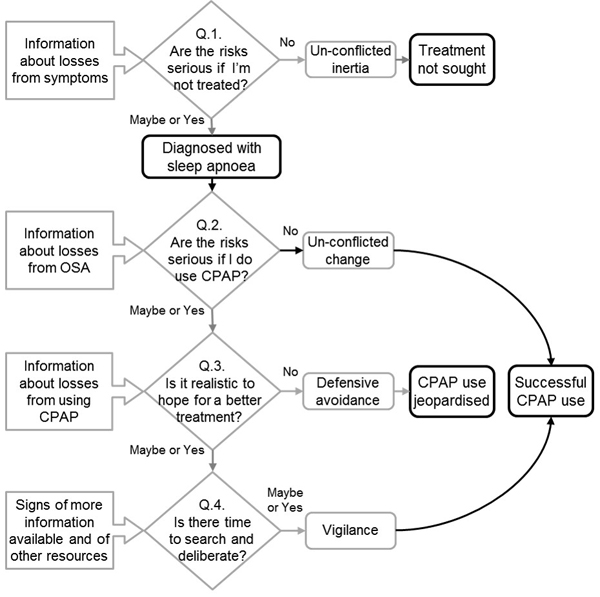
Figure 2: Living with CPAP using JANIS and MANN's decisional conflict model [35]
Yes, no and maybe responses in the above model are based on the decision maker's subjective judgment, not on what is considered best clinical practice. Information about losses from OSA describes what the participants perceived as a loss. This idea corresponds with the sub-category becoming motivated that outlined what participants understood to be the negative consequences of untreated sleep apnoea. Similarly, information about losses from using CPAP corresponds to the side effects and perceived stigma addressed in overcoming and yielding to barriers subcategory. [36]
Un-conflicted change in the above model is congruent with data from participants who reported no hesitation in using CPAP. Each described CPAP as a problem solution that worked; that required little thought and that they "just got on with" because "that's all there is to it!" (P3 and P11). Participants who demonstrated defensive avoidance individually reasoned that by using CPAP for a certain number of hours a night, they could abandon the mask for the remainder of the night. In an attempt to postpone the inevitable need to use CPAP, participants also reasoned that if they lost weight, they might not need CPAP (WARD et al., 2017b, 2018). P17 provided data most consistent with defensive avoidance as the following excerpt illustrates:
"I've been doing other things to try and—like keeping the weight down and trying to do other things, so I don't have to use [CPAP]. It's just the machine is a bit of a pain [laughter]. But I've been that busy I haven't actually been fatigued because I just have to concentrate on what I'm doing. It's like I sort of can try and do without it. ... They [clinic staff] said you should be using it. Otherwise, you'll die, but I don't think I've been stopping breathing so much as I used to. ... Sleep apnoea is a thing that—I've spoken to quite a few people—that you can try and control it yourself. As I say I've dropped a bit of weight—about 4 kilos, which they've said would be a good thing for it. ... I would like to try and be tested again and see what the outcome was for that." [37]
P17 avoided information that conflicted with his belief that losing weight would work as a solution to his sleep apnoea, instead focusing on information that supported his belief about abandoning CPAP. This strategy was consistent with the bolstering of preferred alternatives to diminish cognitive dissonance (RAPOPORT, 1998). [38]
However, the majority of participants exhibited a vigilant coping strategy. Participants weighed the pros and cons of not using CPAP against the pros and cons of using it to determine an optimum course of action. Participants sought further information to determine if it was realistic to hope for an alternative to CPAP. Despite difficulty at the outset, P5, P8 and P9 described a thorough search for information about sleep apnoea and CPAP and were determined to persevere with CPAP use. They took a measured approach to information gathering and the assessment and evaluation of options before making a firm decision to commit to living with CPAP. Indeed, CPAP-users with an un-conflicted change coping style or a vigilant coping style were more likely to persevere and succeed with CPAP than those who favored defensive avoidance. [39]
What the model in Figure 2 does not illustrate is how bargaining and balancing throughout the process of getting used to CPAP led to movement back and forth between defensive avoidance and vigilance. A unique feature of the decisional conflict model is the influence of situational factors that can cause the same person to make a rational decision in one circumstance, but a poor decision in another (WEBER, BARON & LOOMES, 2000). This observation is consistent with findings from this study and the night-to-night variability of CPAP use observed by WEAVER et al. (1997) and others (ALOIA, ARNEDT, STANCHINA & MILLMAN, 2007; PITTSLEY et al., 2005; WOHLGEMUTH et al., 2014; YE et al., 2012). Despite describing consistent CPAP use, participants chose to use or not to use CPAP based on the circumstances of that moment, for example, taking the mask off part way through the night or choosing not to take CPAP while traveling (P6). [40]
Scholars have applied the conflict theory model of decision-making in areas such as education, mental health, human resource management and chronic disease management (BOUCKENOOGHE et al., 2007; DE HEREDIA, AROCENA & GÁRATE, 2004; GRYTTEN et al., 2013; UMEH & OMARI-ASOR, 2011). However, examples of sleep medicine studies using the conflicted decision model are scant. STEPNOWSKY, BARDWELL et al. (2002) identified that an active coping style increased CPAP use, while MORAN et al. (2012) noted an active coping style made little difference to use. Further studies by STEPNOWSKY, MARLER et al. (2002, 2006) explored social cognitive correlates of CPAP use with experienced users and the determinants of nasal CPAP compliance. They concluded that when pros outweighed cons, CPAP use increased. Additionally, CRAWFORD, ESPIE, BARTLETT and GRUNSTEIN (2014) promoted the encouragement of adaptive coping styles. Given that bargaining and balancing reflects this model of decision-making, it would be pertinent to explore its applicability to decision aids for CPAP-users. [41]
Sleep medicine literature has focused on the importance of using CPAP and the problem of the non-compliant CPAP-user. The high personal and economic cost of untreated and under-treated OSA is well documented. In particular, researchers have applied various theoretical models to develop interventions to sustain CPAP use and to identify under-use. Although sleep medicine scholars have used theoretical models to explain non-compliance, scant evidence exists to explain the use of CPAP. One solution to difficulties optimizing CPAP use is to identify how CPAP-users are successful. Bargaining and balancing life with CPAP is a new grounded theory constructed from interview data that is contextualized within change and decision theories and is the first to identify the components of masterful CPAP use. This theory explains how participants bargained and balanced personally, and in close relationship with others, through a process of making choices about CPAP during which they were active, reasoned decision-makers in their healthcare. In this article, we propose that change and decision theories may underpin successful strategies for patients in the context of bargaining and balancing life with CPAP and other long-term treatment. Further research is now warranted to explore these components in more detail. [42]
The theories of change management and decision-making that support the process of bargaining and balancing, both individually and in partnership, underpin the process of integrating CPAP into everyday life. Data from this study offer valuable and targeted information to optimize uptake of this therapy and raise important questions about the relevance of framing CPAP-users as active decision-makers in their care. For example, aligning data from this study with the vigilance coping pattern provides evidence that assessing coping styles in prospective CPAP-users might have predictive value. Education and behavioral medicine researchers have used coping style assessments, based on JANIS and MANN's model, to analyze the decision patterns and decision-making self-esteem of university students. Using coping style assessments gives the opportunity to target supportive interventions at those who relate more closely to less effective coping patterns. Subsequently, interventions that address particular coping styles can be tested to determine the possibility of transitioning CPAP-users from sub-optimal CPAP use to optimizing CPAP use. [43]
Clinical environments that acknowledge and support the social process of bargaining and balancing life with CPAP may be successful in optimizing uptake of this therapy. Each of the theoretical models we have discussed has a degree of congruence with a separate part of the bargaining and balancing process, and so strengthens understanding of long-term therapy use. Moreover, identifying how people have succeeded in becoming used to CPAP provides a source of information for the development of clinical and patient education resources. Therefore, the theory of bargaining and balancing has widespread implications for policy, research and practice. Plans to conduct further research into this theory are being developed in healthcare settings in New Zealand and overseas. [44]
Aloia, Mark; Arnedt, Todd; Stanchina, Michael & Millman, Richard (2007). How early in treatment is PAP adherence established? Revisiting night-to-night variability. Behavioral Sleep Medicine, 5(3), 229-240.
Aloia, Mark; Arnedt, Todd; Stepnowsky, Carl; Hecht, Jackie & Borrelli, Belinda (2005). Predicting treatment adherence in obstructive sleep apnea using principles of behavior change. Journal of Clinical Sleep Medicine, 1(4), 346-353, http://www.aasmnet.org/jcsm/ViewAbstract.aspx?pid=26359 [Accessed: October 15, 2012].
Aloia, Mark; Arnedt, Todd; Strand, Matthew; Millman, Richard & Borrelli, Belinda (2013). Motivational enhancement to improve adherence to positive airway pressure in patients with obstructive sleep apnea: A randomized controlled trial. Sleep, 36(11), 1655-1662.
Barbé, Ferran & Pépin, Jean-Louis (Eds.) (2015). Obstructive sleep apnoea. Sheffield: European Respiratory Society.
Birks, Melanie & Mills, Jane (2015). Grounded theory: A practical guide. Los Angeles, CA: Sage.
Birks, Melanie; Mills, Jane; Francis, Karen & Chapman, Ysanne (2009). A thousand words paint a picture: The use of storyline in grounded theory research. Journal of Research in Nursing, 14(5), 405-417.
Bouckenooghe, Dave; Vanderheyden, Karlien; Mestdagh, Steven & van Laethem, Sarah (2007). Cognitive motivation correlates of coping style in decisional conflict. The Journal of Psychology, 141(6), 605-626.
Boudon, Raymond (2003). Beyond rational choice theory. Annual Review of Sociology, 29(1), 1-21.
Braham, Peter. (2013). Key concepts in sociology. London: Sage.
Brüderl, Josef & Kalter, Frank (2001). The dissolution of marriages: The role of information and marital‐specific capital. The Journal of Mathematical Sociology, 25(4), 403-421.
Charmaz, Kathy (2014). Constructing grounded theory (2nd ed.). Thousand Oaks, CA: Sage.
Clark, Norren & Janevic, Mary (2014). Individual theories. In Kristin Riekert, Judith Ockene & Lori Pbert. (Eds.), Handbook of health behavior change (pp.3-26). New York, NY: Springer.
Crawford, Megan; Espie, Colin; Bartlett, Delwyn & Grunstein, Ron (2014). Integrating psychology and medicine in CPAP adherence—new concepts?. Sleep Medicine Reviews, 18(2), 123-139.
de Heredia, Ramón; Arocena, Francisco & Gárate, José (2004). Decision-making patterns, conflict styles and self-esteem. Psicothema, 16(1), 110-116, http://www.psicothema.com/pdf/1169.pdf [Accessed: August 13, 2015].
Dijkstra, Jan; Lindenberg, Siegwart & Veenstra, René (2007). Same-gender and cross-gender peer acceptance and peer rejection and their relation to bullying and helping among preadolescents: Comparing predictions from gender-homophily and goal-framing approaches. Developmental Psychology, 43(6), 1377-1389.
Fasse, Léonor; Flahault, Cécile; Vioulac, Christel; Lamore, Kristopher; Van Wersch, Anna; Quintard, Bruno & Untas, Aurélie (2017). The decision-making process for breast reconstruction after cancer surgery: Representations of heterosexual couples in long-standing relationships. British Journal of Health Psychology, 22(2), 254-269.
Ghosh, Dipansu; Allgar, Victoria & Elliott, Mark (2013). Identifying poor compliance with CPAP in obstructive sleep apnoea: A simple prediction equation using data after a two week trial. Respiratory Medicine, 107(6), 936-942.
Giles, Tammie; Lasserson, Toby; Smith, Brian; White, John; Wright, John & Cates, Christopher (2008). Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database of Systematic Reviews, 4(Art. No.: CD001106), 1-103.
Goldthorpe, John (1996). The quantitative analysis of large-scale data-sets and rational action theory: For a sociological alliance. European Sociological Review, 12(2), 109-126.
Gordon, Aliza; Wu, Sze-jung; Munns, Nicole; DeVries, Andrea & Power, Thomas (2018). Untreated sleep apnea: An analysis of administrative data to identify risk factors for early nonadherence. Journal of Clinical Sleep Medicine, 14(8), 1303-1313.
Grytten, Nina; Aarseth, J. H.; Espeset, K.; Johnsen, G.; Wehus,R.; Lund, C. & Haugstad,R. (2013). Stoppers and non-starters of disease-modifying treatment in multiple sclerosis. Acta Neurologica Scandinavica, 127(2), 133-140.
Harwood, Lori & Clark, Alexander (2013). Understanding pre-dialysis modality decision-making: A meta-synthesis of qualitative studies. International Journal of Nursing Studies, 50(1), 109-120.
Hillman, David; Murphy, Anita & Pezzullo, Lynne (2006). The economic cost of sleep disorders. Sleep, 29(3), 299-305.
Janis, Irving (1985). Coping patterns among patients with life-threatening diseases. Issues in Mental Health Nursing, 7(1-4), 461-476.
Janis, Irving & Mann, Leon (1976). Coping with decisional conflict: An analysis of how stress affects decision-making suggests interventions to improve the process. American Scientist, 64(6), 657-667.
Janis, Irving & Mann, Leon (1977). Decision making: A psychological analysis of conflict, choice and commitment. New York, NY: Free Press.
Johansson, Lina (2013). Shared decision making and patient involvement in choosing home therapies. Journal of Renal Care, 39(Suppl.1), 9-15.
Kroneberg, Clemens & Kalter, Frank (2012). Rational choice theory and empirical research: Methodological and theoretical contributions in Europe. Annual Review of Sociology, 38(1), 73-92.
Kte'pi, Bill (2013). Decision making, theories of. In K. Bradley Penuel, Matt Statler & Ryan Hagen (Eds.), Encyclopedia of crisis management (pp.247-250). Thousand Oaks, CA: Sage.
Kvale, Steinar & Brinkmann, Svend (2009). InterViews: Learning the craft of qualitative research interviewing (2nd ed.). Los Angeles, CA: Sage.
Marcus, Bess; Eaton, Cheryl; Rossi, Joseph & Harlow, Lisa (1994). Self-efficacy, decision-making and stages of change: An integrative model of physical exercise. Journal of Applied Social Psychology, 24(6), 489-508.
May, Anna; Gharibeh, Tarek, Wang; Lu, Hurley; Amanda, Walia; Harneet, Strohl; Kingman & Mehra, Reena (2018). CPAP adherence predictors in a randomized trial of moderate-to-severe OSA enriched with women and minorities. Chest, 154(3), 567-578.
McEvoy, Doug; Antic, Nick; Heeley, Emma; Luo, Yuanming; Ou, Qiong; Zhang, Xilong; Mediano, Olga; Chen, Rui; Drager, Luciano; Liu, Zhihong; Chen, Guofang; Du, Baoliang; McArdle, Nigel; Mukherjee, Sutapa; Tripathi, Manjari; Billot, Laurent; Li, Qiang; Lorenzi-Filho, Geraldo; Barbe, Ferran; Redline, Susan; Wang, Jiguang; Arima, Hisatomi; Neal, Bruce; White, David; Grunstein, Ron; Zhong, Nanshan & Anderson, Craig (2016). CPAP for prevention of cardiovascular events in obstructive sleep apnea. New England Journal of Medicine, 375(10), 919-931.
McNicholas, Walter T. & Bonsignore, Maria Rosaria (2010). Introduction. In Walter T. McNicholas & Maria Rosaria Bonsignore (Eds.), Sleep apnoea (pp. vii-ix). Sheffield: European Respiratory Society, https://books.ersjournals.com/content/sleep-apnoea-out-of-print [Accessed: August 1, 2015].
Moran, Alicia; Highsmith, Jonathan; Lehockey, Katie & Everhart, Erik (2012). Risk factors and interventions for nonadherence to continuous positive airway pressure (CPAP). In Lisandro Sacchetti & Priscilla Mangiardi (Eds.), Obstructive sleep apnea: Causes, treatment and health implications (pp.1-34). New York, NY: Nova Biomedical.
Opp, Karl-Dieter (1999). Contending conceptions of the theory of rational action. Journal of Theoretical Politics, 11(2), 171-202.
Pittsley, Michelle; Gehrman, Philip; Cohen-Zion, Mairav; Stepnowsky, Carl; Marler, Matthew & Ancoli-Israel, Sonia (2005). Comparing night-to-night variability of sleep measures in elderly African Americans and whites. Behavioral Sleep Medicine, 3(2), 63-72.
Prochaska, James (2013). Transtheoretical model of behavior change. In Marc Gellman & J. Rick Turner (Eds.), Encyclopedia of behavioral medicine (pp.1997-2000). New York, NY: Springer.
Prochaska, James & DiClemente, Carlo (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51(3), 390-395.
Qaseem, Amir; Holty, Jon-Erik; Owens, Douglas; Dallas, Paul; Starkey, Melissa & Shekelle, Paul (2013). Management of obstructive sleep apnea in adults: A clinical practice guideline from the American college of physicians. Annals of Internal Medicine, 159(7), 471-483, http://annals.org/article.aspx?articleid=1742606&resultClick=3 [Accessed: March 26, 2014].
Rapoport, Anatol (1998). Individual psychology of decision-making. In Anatol Rapoport (Ed.), Decision theory and decision behaviour: Normative and descriptive approaches (pp.174-176). London: Palgrave Macmillan.
Sawyer, Amy; Canamucio, Anne; Moriarty, Helene; Weaver, Terri; Richards, Kathy & Kuna, Samuel (2011). Do cognitive perceptions influence CPAP use?. Patient Education & Counseling, 85(1), 85-91.
Sawyer, Amy; Gooneratne, Nalaka; Marcus, Carole; Ofer, Dafna; Richards, Kathy & Weaver, Terri (2011). A systematic review of CPAP adherence across age groups: Clinical and empiric insights for developing CPAP adherence interventions. Sleep Medicine Reviews, 15(6), 343-356.
Scott, John (2000). Rational choice theory. In Gary Browning, Abigail Halcli & Frank Webster (Eds.), Understanding contemporary society: Theories of the present (pp.126-138). London: Sage.
Slovic, Paul; Fischhoff, Baruch & Lichtenstein, Sarah (1977). Behavioral decision theory. Annual Review of Psychology, 28(1), 1-39, http://www.annualreviews.org/doi/abs/10.1146/annurev.ps.28.020177.000245 [Accessed: August 13, 2015].
Smith, Ian; Lasserson, Toby & Haniffa, Muzlifah (2004). Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database of Systematic Reviews, 4(Art. No.: CD003531), 1-81.
Stepnowsky, Carl; Bardwell, Wayne; Moore, Polly; Ancoli-Israel, Sonia & Dimsdale, Joel (2002). Psychologic correlates of compliance with continuous positive airway pressure. Sleep, 25(7), 758-762.
Stepnowsky, Carl; Marler, Matthew & Ancoli-Israel, Sonia (2002). Determinants of nasal CPAP compliance. Sleep Medicine, 3(3), 239-247.
Stepnowsky, Carl; Marler, Matthew; Palau & Brooks, Annette (2006). Social-cognitive correlates of CPAP adherence in experienced users. Sleep Medicine, 7(4), 350-356.
Strauss, Anselm & Corbin, Juliet (1990). Basics of qualitative research: Grounded theory procedures and techniques. Newbury Park, CA: Sage.
Sullivan, Colin; Berthon-Jones, Michael; Issa, Faiq & Eves, Lorraine (1981). Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. The Lancet, 317(8225), 862-865.
Tong, Allison; Lesmana, Brian; Johnson, David; Wong, Germaine; Campbell, Denise & Craig, Jonathan (2013). The perspectives of adults living with peritoneal dialysis: Thematic synthesis of qualitative studies. American Journal of Kidney Diseases, 61(6), 873-888.
Umeh, Kanayo & Omari-Asor, Lorraine (2011). Emotional vulnerability and coping styles for resolving decisional conflict. The Journal of Psychology, 145(4), 297-312.
van Zeller, Mafalda; Severo, Milton; Santos, Ana Cristina & Drummond, Marta (2013). 5-Years APAP adherence in OSA patients—do first impressions matter?. Respiratory Medicine, 107(12), 2046-2052.
Ward, Kim; Hoare, Karen & Gott, Merryn (2014). What is known about the experiences of using CPAP for OSA from the users' perspective? A systematic, integrative literature review. Sleep Medicine Reviews, 18(4), 357-366.
Ward, Kim; Hoare, Karen & Gott, Merryn (2017a). Analysis in grounded theory—how is it done? Examples from a study that explored living with treatment for sleep apnoea. Sage Research Methods Cases, Part 2.
Ward, Kim; Hoare, Karen & Gott, Merryn (2017b). Making choices about CPAP: findings from a grounded theory study. Collegian, 24(4), 371-379.
Ward, Kim; Hoare, Karen & Gott, Merryn (2018). Becoming a team: Findings from a grounded theory study about living with CPAP. Collegian, 25(1), 81-88.
Weaver, Terri; Maislin, Greg; Dinges, David; Younger, Joel; Cantor, Charles; McCloskey, Susan & Pack, Allan (2003). Self-efficacy in sleep apnea: Instrument development and patient perceptions of obstructive sleep apnea risk, treatment benefit, and volition to use continuous positive airway pressure. Sleep, 26(6), 727-732.
Weaver, Terri; Kribbs, Nancy Barone; Pack, Allan; Kline, Lewis; Chugh, Deepak; Maislin, Greg; Smith, Philip; Schwartz, Alan; Schubert, Norman; Gillen, Kelly & Dinges, David (1997). Night-to-night variability in CPAP use over the first three months of treatment. Sleep, 20(4), 278-283.
Weber, Elke; Baron, Jonathan & Loomes, Graham (2000). Conflict and tradeoffs in decision making. New York, NY: Cambridge University Press.
Wild, M.; Engleman, H.; Douglas, N. & Espie, C. (2004). Can psychological factors help us to determine adherence to CPAP? A prospective study. European Respiratory Journal, 24(3), 461-465, https://erj.ersjournals.com/content/24/3/461.full [Accessed: June 15, 2015].
Wohlgemuth, William; Chirinos, Diana; Domingo, Samantha & Wallace, Douglas (2014). Attempters, adherers, and non-adherers: Latent profile analysis of CPAP use with correlates. Sleep Medicine, 16(3), 336-342.
Wozniak, Dariusz; Lasserson, Toby & Smith, Ian (2014). Educational, supportive and behavioral interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database of Systematic Reviews, 1(Art No.: CD007736), 1-94.
Ye, Lichuan; Pack, Allan I.; Maislin, Greg; Dinges, David; Hurley, Sharon; McCloskey, Susan & Weaver, Terri (2012). Predictors of continuous positive airway pressure use during the first week of treatment. Journal of Sleep Research, 21(4), 419-426.
Kim WARD is a registered nurse and lecturer at the University of Auckland's School of Nursing specializing in patients' experiences of long-term conditions to inform practice and interventions, primarily in sleep medicine. She has a background in intensive care and respiratory nursing and completed her doctorate exploring experiences of using therapies for sleep apnoea. She is a qualitative researcher, currently exploring patient experience and the function of partners in improving patient outcomes in the areas of sleep medicine and long-term therapies. Research interests include patients' experiences of healthcare and qualitative methodologies, particularly grounded theory and mixed methodology.
Contact:
Kim Ward
School of Nursing
The University of Auckland
85 Park Road, Grafton
Auckland, New Zealand
Tel.: +64 9 923 3119
E-mail: k.ward@auckland.ac.nz
URL: https://unidirectory.auckland.ac.nz/profile/k-ward
Merryn GOTT is a professor at the University of Auckland's School of Nursing and a palliative care and gerontology research specialist who has been conducting research with older people for over 20 years. She has a particular interest in developing models of palliative and end of life care to meet the needs of ageing populations. Merryn directs the Te Arai Palliative Care and End of Life Research Group. The group conducts multi-disciplinary bicultural research using creative social research methods to inform practice, policy, and teaching in palliative and end of life care both nationally and internationally.
Contact:
Merryn Gott
School of Nursing
The University of Auckland
85 Park Road, Grafton
Auckland, New Zealand
Tel.: +64 9 923 1655
E-mail: m.gott@auckland.ac.nz
URL: https://unidirectory.auckland.ac.nz/profile/m-gott
Karen HOARE is an associate professor at Massey University and works as a nurse practitioner for children and young people in general practice in South Auckland. She is director of the postgraduate program in the School of Nursing. Her research interests include child and youth health, new graduate nurses in primary care and children's perceptions of issues in the developing world. She has published several articles relating to constructivist grounded theory methodology.
Contact:
Karen Hoare
College of Health, School of Nursing
Massey University
Albany Expressway (SH17)
Auckland, New Zealand
Tel.: +64 9 2127034
E-mail: K.J.Hoare@massey.ac.nz
Ward, Kim; Gott, Merryn & Hoare, Karen (2019). Mastering Treatment for Sleep Apnoea: The Grounded Theory of Bargaining and Balancing Life With Continuous Positive Airway Pressure (CPAP), in the Context of Decisional Conflict and Change Theories [44 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 20(3), Art. 13, http://dx.doi.org/10.17169/fqs-20.3.3137.