

Volume 9, No. 1, Art. 8 – January 2008
Conflicting Obligations: Role Conflict Among Health Care Complaints Managers
Clare Xanthos
Abstract: This article draws on selected findings from a study which explored the conflicts and tensions inherent in the role of UK National Health Service (NHS) complaints managers. It is argued that balancing loyalties to the complained about health service organisation against the needs of complainants leads to an inherent contradiction in the role of the complaints manager. This proposition is supported by theoretical literature on complaints handlers, administrators and social actors drawn from three social science disciplines: socio-legal studies, public administration and sociology/social psychology.
The study was conducted between 1999 and 2002 in the London/South East region of the UK and uses a qualitative approach. It is based on in-depth telephone interviews recorded with thirty NHS complaints managers. The focus here is on the interviews conducted with twenty-one of these complaints managers (those complaints managers who worked in NHS hospitals as opposed to the primary care sector). Three key areas emerged as the principal findings of the research: 1. The complaints manager's role encompasses inherent contradictions; 2. complaints managers exhibited very different responses/reactions to the inherent contradictions in their role; 3. there were different types of complaints managers. This article focuses on the first finding, that is, the complaints manager's role encompasses inherent contradictions.
Key words: health care complaints, National Health Service (NHS), NHS complaints, NHS complaints procedure, NHS complaints managers, role conflict
Table of Contents
1. Introduction
2. The Inherent Contradiction in the Role of the NHS Complaints Manager
2.1 Socio-legal framework
2.2 Public administration framework
2.3 Sociological and social psychological framework
3. Methods
3.1 Informed consent and anonymity
3.2 Data collection
3.3 Data analysis
4. Results
4.1 Difficulties with consultants
4.2 Differences of opinion between the complaints manager and other staff
4.3 Dealing with conflicting accounts
5. Discussion
Appendix 1: Complaints Manager Interview Guide
Most health care in the UK is delivered by the publicly funded health care system, the National Health Service (NHS), founded in 1948. The NHS has a complaints procedure where patients and their families can file complaints about NHS health care providers. The "NHS complaints manager" is a key player in the NHS complaints procedure as complaints managers are the staff group with the most comprehensive overview of the operation of the complaints procedure (DEPARTMENT OF HEALTH, 2001). Complaints managers are of particular significance because they oversee the administrative decision-making process at the initial stage of the complaints procedure in which the vast majority of complaints are dealt with. [1]
Of particular interest is the fact that complaints managers operate in an environment which is often defensive towards complainants (see LLOYD-BOSTOCK, 1992; BRISTOL ROYAL INFIRMARY INQUIRY, 2001); at the same time complaints managers have a duty to complainants to handle complaints impartially. It could be argued that the conflict between loyalty to the organisation and the requirement to handle complaints impartially, leads to an inherent contradiction in the complaints manager's role. [2]
Additionally, a key shortcoming of the academic literature on health service complaints has been the scarcity of both theoretical and empirical work on the role of complaints handlers, especially on the conflicts in the role played by organisation complaint handlers (see MULCAHY, LICKISS, ALLSOP & KARN, 1996). Thus, we do not yet have a satisfactory explanation of health service complaints handlers which specifically explores the conflicts and tensions in their role. As such, there was a gap in the literature which was the intention of this study to fill. [3]
This article then will explore the proposition that there is an inherent contradiction in the role of the NHS complaints manager due to the likelihood that complaints managers are caught between loyalties to the organisation and the requirement to handle complaints impartially. [4]
2. The Inherent Contradiction in the Role of the NHS Complaints Manager
This article utilises an interdisciplinary conceptual framework for exploring the inherent contradiction or conflict in the role of NHS complaints managers, drawing from a number of social science disciplines: socio-legal studies, public administration, and sociology/social psychology. [5]
The socio-legal literature provides a framework for understanding the role of the NHS complaints manager in relation to being a complaints handler or third-party dispute handler. [6]
From this perspective, it can be argued that there is a conflict of interest in the role of an "in-house" complaints handler as there would be concerns that working in the complained about organisation might cause professional loyalties to override fair play (see DEPARTMENT OF HEALTH, 1994). [7]
In theory at least, complaints handlers and third-party dispute handlers are expected to deal impartially with a dispute and are expected to be independent. MULCAHY and LLOYD-BOSTOCK (1994) point out that an essential characteristic of both arbitration and adjudication is that an independent third party whose interests are not related to either of the parties hears the dispute. However, various socio-legal scholars point out that in actuality, complaints handling is far from independent (see NADER, 1980; BLACK & BAUMGARTNER, 1983). NADER argues that without the law as a back up, third-party complaint handlers are of limited use; she makes the case that if the party resolving the case is also the party being complained against, the odds of the complainant achieving success are small (NADER, 1980). Similarly, BLACK and BAUMGARTNER (1983) state that many third parties who claim to be neutral in a conflict are actually biased in favour of one side or the other. More recently, MULCAHY (2001) makes the case that the concept of neutrality as illustrated in adjudication and mediation literature is not an empirical possibility (2001, p.506), and that inequality exists in all disputes and interactions to a certain extent (2001, p.523). [8]
It could be argued then that while in-house complaints systems may pay lip-service to the language of impartiality and independence, in practice impartiality and independence are unlikely. As such, paying lip-service to the rhetoric of impartiality in a system that lacks impartiality is likely to produce contradictions or conflicts for the complaints handlers operating the system. [9]
2.2 Public administration framework
The public administration literature provides a framework for understanding the role of the complaints manager in the broader sense of an administrator employed in a public service. Thus, as well as being complaints handlers, complaints managers are administrators/employees of bureaucracies. [10]
From this perspective, it could be argued that there is a conflict between the organisational agenda and duty to the public. In other words, the demands of the organisation play a key role in the behaviour of public administrators (see VAN WART & DENHARDT, 2001); at the same time, the modern public service requires that administrators perform their duties not only with reference to organisational efficiency but with reference to their own morality and obligations to service users (see COOPER, 2001). In the book "The Responsible Administrator", Terry COOPER (1990) uses the concept of "conflicts of authority" to explain conflicts between two or more objective responsibilities imposed by two or more sources of authority, such as organisational supervisors and the public. COOPER reasons that the imposition of dual responsibilities, which demand incompatible actions, can lead to the individual feeling torn between the two sources of authority. He explains: "'Damned if you do, damned if you don't' is a common way of expressing this feeling of being caught between incompatible alternatives" (1990, p.83). [11]
Thus, employees who attempt to place duty to the public above the orderly operation of his/her organisation are invariably viewed as a serious threat (COOPER, 1990); although it is possible for administrators to choose not to be blindly loyal to the organisation, and to instead choose to follow the values of society and the moral order, this often means considerable sacrifice, such as the loss of job, wages, and status associations (DENHARDT, 1988). For these reasons, it is clear that adherence to the values of duty to the public can be a highly problematical stance for the administrator working in a public organisation such as the NHS. [12]
2.3 Sociological and social psychological framework
The sociological and social psychological literature provides a framework for understanding the role of the complaints manager in relation to the concept of role conflict. Thus, as well as being complaints handlers and administrators, NHS complaints managers can be conceptualised as actors in the social system. This conceptualisation of the complaints handler's role is clearly much broader than the two previous frameworks; indeed, the concept of role is one of the most popular ideas in the social sciences, and provides a framework for discussing or studying many social issues (BIDDLE, 1986). [13]
From this perspective, each social status (position) involves a number of different roles (MERTON, 1957) which means that there is a potential for conflict between these different roles. Indeed, role conflict can manifest itself in a number of ways; first, it can be explained in terms of incompatible roles where an individual might have two roles, which are not compatible with each other; second, it can be explained as conflicting expectations from different groups of people; third it can be explained as a conflict between a designated role and personality, that is, when the behaviours called for by others do not fit the self-concept of the role enactor (see ARGYLE, 1983). [14]
Role conflict has particular relevance to the study of organisations in that staff may be involved in an occupational role, which is at odds with their organisational expectations and demands (see SALAMAN, 1980). As such, workers will routinely experience conflict and frustration within their employing organisation (see SALAMAN, 1980; GOODE, 1960). [15]
This article draws on interview data from a study on the conflicts and tensions of NHS complaints managers which was conducted in the London/South East region of the UK. It focuses primarily on findings from qualitative telephone interviews with twenty-one complaints managers working in NHS hospitals (the original study included interviews with thirty complaints managers working in both hospitals and health authorities, as well as two other methods of data collection)1). [16]
The participants were selected randomly from the North Thames and South Thames NHS directories.2) Seventy-nine complaints managers made up the initial sample. The final sample consisted of thirty complaints managers (twenty-one working in hospitals and nine working in health authorities). [17]
3.1 Informed consent and anonymity
In line with the general principles of informed consent, respondents explicitly indicated their willingness to participate in the study. Formal consent was obtained from participants by using a form which was attached to the letter requesting the interview, to be returned by complaints managers stating they were/were not prepared to be interviewed. Also, with regard to information supplied to respondents, subjects were made aware of the purpose of the study, the extent of their involvement (i.e. the approximate time required to conduct the interviews) and the proposed use to which the findings would be put (i.e. that the study was related to the researcher's PhD thesis). Additionally, in relation to issues of confidentiality and anonymity, it was made clear to respondents that all information provided by them would be treated as confidential and no individual organisation would be identifiable. It was emphasised that anything said by the respondents would be reproduced in an anonymised form in the PhD thesis/any publication generated by the study. In addition, respondents were asked whether it would be acceptable to tape the interview before the interview began. [18]
While the data for the entire study was collected between 1999 and 2002, the data from which this article draws (twenty-one complaints manager interviews) was collected over a two-month period (July and August 1999). These were audio-taped and fully transcribed during September 1999. Interviews lasted approximately one hour. [19]
The interviews explored the contradictions inherent in the role of the complaints manager and how complaints managers responded to this contradiction. In terms of the material covered in this article, a number of questions (see Appendix 1 for Complaints Manager Interview Guide) explored the contradiction in the complaints manager role with particular reference to the complaints investigation. This group of questions aimed to delve into any difficulties in extracting information regarding complaints. How did complaints managers, for example, deal with the probable defensiveness of complained about staff? This question was significant as complaints managers had direct responsibility for the coordination of complaints investigations. Not surprisingly, these questions tended to be sensitive because they required complaints managers to discuss conflicts with members of their own organisations (as opposed to complainants). Hence, these questions required considerable care and were designed to be as non-threatening as possible. For example, the following question explored a positive aspect of the complaints manager's role in order to encourage them to talk about any problems with complaints investigations: "Do you need special skills to obtain necessary information regarding complained about staff?" [20]
Much qualitative analysis falls under the general heading of "thematic analysis" (LACEY & LUFF, 2001). OLESEN, DROES, HATTON, CHICO, and SCHATZMAN (1994) draw attention to the importance of being flexible and of being open to mixing analytic styles and modes. Additionally, PATTON (1990) argues that since each qualitative study is unique, the data analytical approach used will similarly be unique. In this vein, the data analysis of the complaints manager interviews was not guided by a specific analytical approach; rather the data analysis evolved in response to the development of the work in progress. In keeping with the general purpose of qualitative data analysis, the aim was to make sense of the data produced by reducing the volume of information, identifying significant patterns, and constructing a framework for communicating the essence of what the data revealed (PATTON, 1990). [21]
At the same time, the analysis of the complaint manager interviews shares some of the features of grounded theory analysis. After familiarization with the material, certain ideas emerged in the transcript (see LACEY & LUFF, 2001). It was then possible to draw out a number of patterns. In addition, the process of data analysis for the complaints manager interviews was cumulative and involved frequent revisiting of data in the light of the new analytical ideas that emerged as data collection and analysis progressed (see LACEY & LUFF, 2001). Moreover, the final proposition of the research was grounded in both the data that had been collected and the conceptual framework of the study (see MASON, 1994). Thus, the coding system (see Appendix 2) derived from the interview data was subsequently linked to the original proposition; in other words, all the themes which were identified were related to the proposition that there was an inherent contradiction in the complaints manager's role3). As such there was an interplay between the coding system derived from the data and the conceptual framework (see BULMER, 1984). [22]
Readers should be aware that while the results as described below correspond with the original proposition and may appear to have been generated through the literature alone, in fact, this proposition is equally informed by the empirical data. In other words, the proposition was not defined a priori. Thus, at the beginning of the study, a review of the literature led to the identification of the proposed project. In turn the findings and subsequent data analysis led to searching for additional literature which explained the data, and so on. Accordingly, the theoretical literature and the empirical data are closely intertwined (as described above). This is in keeping with Michael PATTON's observations that qualitative inquiry designs cannot be completely specified in advance of fieldwork; a qualitative design unfolds as fieldwork unfolds (1990, p.61). In a similar vein, RUBIN and RUBIN (1995, p.41) suggest that the qualitative researcher needs to have a high tolerance for uncertainty, especially at the beginning of the project, because the design will continue to change as the researcher makes sense of the data. [23]
Complaints manager interviews indicated that there was an inherent contradiction in the complaints manager role in terms of investigating complaints while being an employee of the complained about organisation. [24]
4.1 Difficulties with consultants
A number of complaints managers remarked that communicating with complained about staff was made especially difficult if there were marked differences in hierarchy between the complaints manager and the complained about staff. Nearly half of the complaints managers referred to the problems associated with difficult hospital consultants.4) One complaints manager commented:
"… There's still a couple [of consultants] who are defensive and do bury their head in the sand—and I have terrible trouble actually getting a response out of them." [25]
Another respondent linked the attitude of some consultants with the culture of the medical profession:
"… probably a quarter [of consultants] I have a problem with—but then they are probably a problem for everybody! …There is such a big change in the NHS—and even just in health care generally—I mean years and years ago, you never questioned the doctor's word—and I think it's very, very hard for doctors now … they are more answerable … and I think some of them have a real difficulty in being answerable." [26]
It emerged from interviews that complaints managers often dealt with consultants more easily if the complaints manager had a reasonably high status in the organisation. For this reason, some respondents felt that complaints managers and investigating staff needed sufficient clout to obtain information from complained about staff. A "high level" complaints manager (also the deputy chief executive) explained:
"You will see … that there is a requirement that there is a designated complaints manager, and that the complaints manager is at a sufficient level in the organization to carry some clout—either reporting directly to the Chief Executive, or pretty close. I think if you had somebody who was sort of in an admin grade and maybe was pretty young and inexperienced, I think it could be quite daunting—especially when you are dealing with consultants. I mean they can be very arrogant and difficult creatures, and I'm of sufficient status and age and experience—I talk to them at the same level, you know …" [27]
However, most complaints managers were not in posts at the level of the aforementioned respondent. Accordingly, complaints managers often sought help from senior staff when complained about staff obstructed investigations. Some respondents spoke of enlisting the help of Medical Directors if communicating with complained against staff proved problematic. One young complaints manager had approached consultants directly in relation to complaints investigations when she was first appointed to the job. However, when this proved difficult, she enlisted the help of more senior staff:
"If it was a complaint about the attitude of one of the consulting staff, I would definitely go to the Medical Director. I would not confront them at all. Attitude and communication issues I find are the touchiest complaints to discuss … when I was first here ... I would go and speak to staff about it directly. If you put yourself in my shoes, they had this young girl coming to talk to them about their attitude—and I would be pissed off with someone doing that to me. I just became very nervous about doing that. I was young—I put consultants and doctors up on a pedestal—I thought, 'this is awful—I can't do it.'" [28]
She acknowledged that she would find the job impossible without support from the Medical Director. When asked what she thought it would be like for complaints managers who did not have sympathetic Nursing Directors or Medical Directors, she replied with feeling:
"It must be awful—if I was in that position, I don't think I would stay—It would be incredibly difficult I am sure—I think you would have to be a very strong person to be able to stand up to that every single day." [29]
Another respondent similarly acknowledged that he enlisted the help of the Medical Director when necessary:
"I put the Medical Director on to them—they're scared of him because he's a bit of a terrier—he doesn't mince his words, which is great—it's really helpful for me." [30]
4.2 Differences of opinion between the complaints manager and other staff
Nearly half of the complaints managers acknowledged differences of opinion of how to handle complaints with other staff. Complaints managers frequently had differences of opinion on handling particular complaints, with senior management staff, for example, the Director of Nursing and the Medical Director. One respondent spoke candidly about his plea for an independent investigation being refused by a Director of Nursing:
"… I've had a couple of differences with say the Director of Nursing … a couple of times when I've said, 'I think this ought to go out for an independent investigation to whoever', and she's disagreed with me and overruled me—but that's OK—it happens. There was one particular one I was very concerned about—I wasn't happy at all—and I said to the Director of Nursing … 'I would like an independent report from such and such a person.' She said, 'no, I don't think we need to do that …'" [31]
Additionally, a couple of complaints managers spoke of difficulties or awkwardness with staff (both service managers and complained about staff) with regard to producing letters to complainants with appropriate apologies, due to staff opposition to apologies. One complaints manager reported staff resistance to incorporating an apology into the "acknowledgement letter" to complainants. She, personally, felt strongly that the letter should include an apology, and insisted on its inclusion, despite staff objections:
"A lot of staff get very upset about us putting an apology in the letter … In the acknowledgement letter, a lot of staff get upset that we apologize 'for any distress that you feel you have been caused.' They feel we shouldn't put that in … I think to acknowledge it without putting in some form of apology would actually make people very angry because they would think, 'well, they just don't care.' … When I first came and sort of changed a lot of the letters—I feel very strongly that people should have an apology—and so I was very adamant about that—and that went in and that stayed in." [32]
In a similar vein, in relation to "final response letters", another complaints manager explained:
"I feel, for me, I need to be able to put myself in the position of the complainant, and write a response that deals with every issue in a sympathetic way, even if the staff who have done the investigation have said, 'well this is a totally ridiculous complaint and of course things didn't happen like that.' … and we do say things like 'I am sorry if your perception was ...' or 'if you felt that'... and often—yes … staff criticize that. They feel that what we're writing is more for the patient than for them ... I mean I am criticized for doing it by staff …" [33]
4.3 Dealing with conflicting accounts
Complaints investigations invariably generated conflicting accounts from both sides which put complaints managers in an automatic dilemma. As one interviewee explained:
"... It's very difficult when it's a conversation that's been had without witnesses, on a one-to-one basis, and the complainant is saying one thing, and the nursing staff are saying another thing." [34]
Two-thirds of the complaints managers acknowledged that there were occasions when they doubted whether they were receiving the complete picture of the circumstances of the complaint from complained about staff and/ or investigating staff. In this situation, complaints managers are confronted with significant dilemmas in that they are coordinating complaints investigations while being a member of the organisation complained about. Do they reluctantly accept the staff account, or do they try to influence relevant persons to ensure an impartial investigation? The question of what to do, in the event of conflicting accounts from the complainant and complained about staff, then could be argued to be at the heart of the impartiality issue. [35]
COOPER (1990) has highlighted the pressure to conform in organisations. He observes that any employee who attempts to exercise ethical autonomy by placing loyalty to the greater public good above the orderly operation of the organisation is invariably viewed as a troublemaker. Empirical findings illustrate this issue. Interviews revealed that accepting the complainant's story could make one unpopular. A complaints manager observed:
"Sometimes you have to come to a conclusion that staff may not necessarily like … I am sure I wouldn't win any popularity contests …!" [36]
DENHARDT (1988) contends that organisational reward systems encourage loyalty to the organisation and promote identification with the organisation. The "organisational participant" is likely to suppress personal and social values when this conflicts with the norms encouraged in the organisation. The empirical findings were consistent with this argument. Respondents rarely mentioned accepting the complainant's point of view. Many of the responses showed that complaints managers sided with staff, if there was a lack of evidence to validate complainants' claims. Despite the sensitivity of this issue, over a third of the complaints managers acknowledged directly or indirectly that, ultimately, they would support staff. Indeed, some complaints managers were quite open about siding with staff in the event of conflicting stories:
"It's a thorny one ... the bottom line is—you give staff the benefit of the doubt in the absence of other information, because if you don't give them the benefit of the doubt, you have to take them through a disciplinary. If you take them through a disciplinary, and you don't have sufficient evidence, then you are potentially shafting someone's career." [37]
Similarly the following respondent explained:
"... We have to say, 'this is what our staff are saying, and we are sorry if you are saying something different'—but we have to represent our staff as well as the patient—we work for the hospital. It is very, very difficult. It causes us quite a lot of tension and stress, trying to be fair to all people—but—I suppose at the end of the day, we would come down on the side of staff. You don't want to be seen to not be backing up your staff. Sounds awful that—doesn't it?" [38]
She went on to express further unease about this stance:
"… I don't know what we can do about that—it's actually something I'm starting to think more and more about at the moment, and it's something that I don't know what we can do—but it's something I would like to try and get to the bottom of—try and do something about." [39]
This research clearly suggests that NHS complaints managers are faced with the necessity of reconciling loyalty to the organisation with obligations to complainants and that this represents an inherent contradiction in their role. This contradiction has been explored here with reference to complaints managers' experiences in coordinating complaints investigations. [40]
Nearly half the complaints managers specifically referred to problems with investigations that were caused by difficult consultants; the interviews indicated that the status of the complaints manager had an impact on negotiating with staff, in terms of complaints managers often not possessing the authority to persuade members of staff to cooperate in investigations. Additionally, a similar number of complaints managers acknowledged differences of opinion with other staff on how to handle complaints. Further, the issue of dealing with conflicting accounts was an especially difficult and complex task for complaints managers. Two-thirds of the complaints managers acknowledged that there were occasions when they did not feel that they were getting the full picture of the situation from complained about staff /investigating staff. Despite this, over a third of the respondents made it clear directly or indirectly that ultimately they would side with staff in conflicting accounts. [41]
While it is acknowledged that not all complaints managers experienced difficulties coordinating investigations, essentially the research demonstrates that there is a potential for contradictions or conflict in the role. [42]
Ultimately, the findings show that coordinating complaints investigations can put the complaints manager in direct conflict with the organisational agenda. Whether it is coping with difficult complained about staff such as consultants, dealing with differences of opinion on complaints handling, or grappling with an organisational culture, which seemingly requires that one must back the organisation in the absence of substantial evidence, complaints managers are acutely caught between organisational loyalty and duty to complainants. [43]
The research also indicates that health care organisations need to ensure that complaints handlers are given the necessary authority to consult with health service staff with reference to complaints investigations. Additionally, the finding that complaints managers are under considerable pressure to take on an organisation-oriented approach is influenced by a lack of independence in the complaints system. As such, health care organisations would do well to explore ways of making their complaints systems more independent so as to reduce the conflicts of interest inherent in complaints handling. [44]
Appendix 1: Complaints Manager Interview Guide
A. Background
What is the official title of your post?
Level of post in the organisation?
Background to post?
Type of organisation, i.e. Health Authority5) or Trust6), type of Trust
Length of time in the post
B. The complaints manager and the complainant
Does your job remit include supporting patients in their complaint—or is it purely investigating the complaint/fact-finding? If yes, how far can you go in supporting the patient with their complaint?
Is it easy to maintain neutrality?
Do you ever feel the complainants have unrealistic expectations? Do you ever feel complaints are unjustified? If yes, how do you deal with these types of complaints?
Do ever identify with the complainant? Roughly, how often?
Are you personally affected by any of the complaints—if you hear a particularly bad case?
Do you ever identify with the staff complained about—do you feel sorry for them? Roughly, how often?
C. The complaints manager and the organisation
Is it difficult having to investigate complained about staff?
Do you need special skills to obtain necessary information regarding complained about staff (for final response letter)?
Are there difficulties in obtaining this information? If yes, how do you get around these difficulties?/Any other ideas?
Are there occasions when you get conflicting stories from the complainant and the complained about staff? How do you feel about this? If yes, what generally happens in this situation?
Are there occasions when you don't feel you are getting the full picture of the situation from complained about staff/investigating staff? What do you do?
Do you have differences of opinion of how to handle complaints with other complaint handling staff (for example, medical directors, nursing directors)? Are there occasions when you have come to a conclusion about a complaint, but another/other members of staff do not accept it?
Are there any occasions when you feel the complainant should be given certain information, but because of rules and regulations you cannot divulge this information?
Do you get the same complaints coming up again and again about the same member of staff/unit/ward (and so on)?
Do you ever feel you would like to be more proactive about complaints than your job/the rules/regulations allows? Do you ever feel your hands are tied?
Does the organisation have a mechanism by which lessons are learned by complaints i.e. the quality of the service is improved through complaints monitoring and analysis? Do you think this is enough?
D. Other questions
What do you think of the complaints system in terms of fairness/justice for the complainant?
Is your post more stressful than the typical managerial job? If yes, what are the key problems/stresses?
If a Mental Health Trust, do you think the mental health aspect of this Trust affects your post? If yes, how?
If a Mental Health Trust, do you think complaints managers working in Mental Health Trusts need additional training?
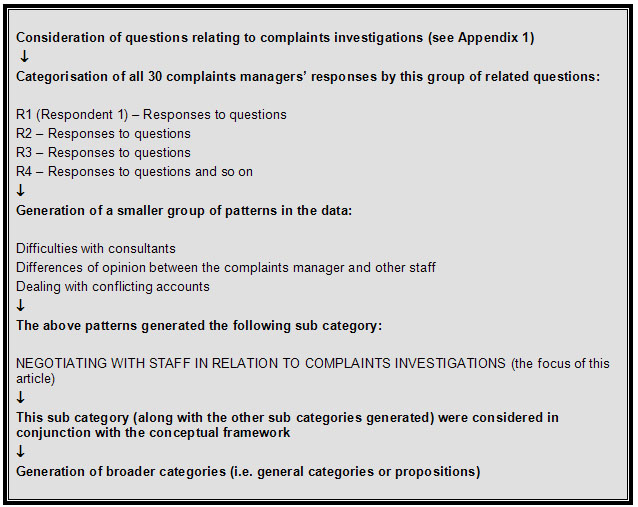
Box 1: Fitting data into sub-categories7) and general categories (Example)
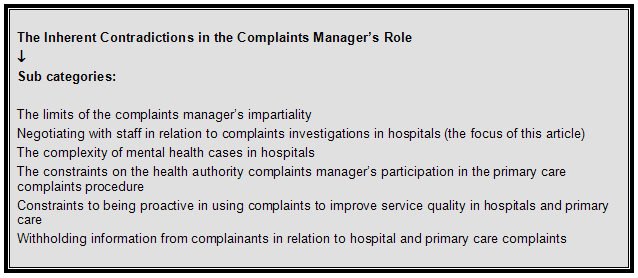
Box 2: A general category8)
1) In the original study, the complaints manager interviews were supplemented with documentary analysis of job descriptions and person specifications of complaints managers and e-mail interviews with "complaints experts" (professionals who were not complaints managers, but had a specialist knowledge of the complaints manager role). <back>
2) Health service directories for the London and Outer London NHS regions. <back>
3) While this article focuses on one theme, that is, the specific contradiction in the complaints manager role with regard to complaints investigations, a number of themes relating to the contradiction in the complaints manager role were coded/identified, for example, another theme that was uncovered was the complexity of mental health cases. <back>
4) The uncooperative behaviour of consultants is consistent with research carried out on doctors’ responses to complaints. MULCAHY (1996) reports that a number of consultants felt that it was not a manager’s place to handle complaints about clinical matters and thus managerial input to complaints was often made impossible. <back>
5) Primary care sector <back>
6) Hospital <back>
7) The basic framework for generating a sub category was one question per sub category, however, some questions generated more than one sub category, and as in the given example, one sub category could be generated from more than one question. <back>
8) This stage of data analysis involved fitting all the sub categories (generated from the interview transcripts) into appropriate general categories (generated from the conceptual framework in conjunction with the sub categories). The linking of sub categories (drawn from the empirical data) to general categories (generated from the conceptual framework and empirical data) in this way directly relates the empirical findings to the conceptual framework. All the sub categories fitted into one of two general categories (i.e. propositions or themes). These were:
the inherent contradictions in the complaints manager’s role (the focus of this article);
complaints managers’ responses and reactions to the contradictions in their role. <back>
Argyle, Michael (1983). The psychology of interpersonal behaviour. Harmondsworth: Penguin Books.
Biddle, Bruce (1986). Recent developments in role theory, Annual Review of Sociology, 12, 67-92.
Black, Donald & Baumgartner, Mary (1983). Towards a theory of the third party. In Keith Boyum & Lynn Mather (Eds.), Empirical theories about courts (pp.84-114). New York: Longman.
Bristol Royal Infirmary Inquiry (2001). Learning from Bristol: The report of the public inquiry into children's heart surgery at the Bristol Royal Infirmary 1984-1995. London: The Stationery Office.
Bulmer, Martin (1984). Concepts in the analysis of qualitative data. In Martin Bulmer (Ed.), Sociological research methods (2nd edn., pp.241-262). London: Macmillan Publishers Ltd.
Cooper, Terry (1990). The responsible administrator: An approach to ethics for the administrative role. San Francisco: Jossey-Bass Inc.
Cooper, Terry (2001).The emergence of administrative ethics as a field of study in the United States. In Terry Cooper (Ed.), Handbook of administrative ethics (pp.1-36). New York: Marcel Dekker.
Denhardt, Kathryn (1988). The ethics of public service: resolving moral dilemmas in public organizations. Connecticut: Greenwood Press.
Department of Health (1994). Being heard: The report of a review committee on NHS complaints procedures (chair: Professor Alan Wilson). London: HMSO.
Department of Health (2001). NHS complaints procedure national evaluation. London: Department of Health.
Goode, William (1960). A theory of role strain. American Sociological Review, 25, 483-496.
Lacey, Anne & Luff, Donna (2001). Trent Focus for research and development in primary health care: An introduction to qualitative analysis. Trent Focus.
Lloyd-Bostock, Sally (1992). Attributes and apologies in letters of complaint to hospitals and letters of response. In John Harvey, Terri Orbuch & Ann Weber (Eds.), Attributions, accounts and close relationships (pp.209-220). New York: Springer-Verlag.
Mason, Jennifer (1994). Linking qualitative and quantitative data analysis. In Alan Bryman & Robert Burgess (Eds.), Analyzing qualitative data (pp.89-110). London: Routledge.
Merton, Robert (1957). The role-set: Problems in sociological theory. British Journal of Sociology, 8(2), 106-120.
Mulcahy, Linda (1996). From fear to fraternity: Doctors' construction of rational identities in response to complaints. Journal of Social Welfare & Family Law, 18(4), 397-412.
Mulcahy, Linda (2001). The possibilities and desirability of mediator neutrality—towards an ethic of partiality? Social & Legal Studies, 10(4), 505-527.
Mulcahy, Linda & Lloyd-Bostock, Sally (1994). Managers as third-party dispute handlers in complaints about hospitals. Law & Policy, 16(2), 196.
Mulcahy, Linda; Lickiss, Rachel; Allsop, Judith & Karn, Valerie (1996). Small voices, big issues: An annotated bibliography of the literature on public sector complaints. London: University of North London Press.
Nader, Laura (1980). Alternatives to the American judicial system. In Laura Nader (Ed.), No access to law: Alternatives to the American judicial system (pp.3-55). New York: Academic Press
Olesen, Virginia; Droes, Nelle; Hatton, Diane; Chico, Nan & Schatzman, Leonard (1994). Analyzing together: Recollections of a team approach in analysis. In Alan Bryman & Robert Burgess (Eds.), Analyzing qualitative data (pp.111-128). London: Routledge.
Patton, Michael (1990). Qualitative evaluation and research methods. California: Sage Publications.
Rubin, Herbert & Rubin, Irene (1995). Qualitative interviewing: The art of hearing data. California: Sage Publications.
Salaman, Graeme (1980). Roles and rules. In Graeme Salaman & Kenneth Thompson (Eds.), Control and ideology in organisations (pp.128-152). Milton Keynes: The Open University Press.
Van Wart, Montgomery & Denhardt, Kathryn (2001). Organizational structures as a context for organizational ethics. In Terry Cooper (Ed.), Handbook of administrative ethics (pp.227-241). New York: Marcel Dekker.
Dr. Clare XANTHOS is a social policy specialist with particular expertise in the areas of health care and housing. Dr XANTHOS attained her PhD in Social Policy from the London School of Economics and Political Science in 2004. Her doctoral research, which was highlighted in "The Times" (20/9/05) was titled "NHS Complaints Managers: A Study of the Conflicts and Tensions in their Role". She also holds a Masters degree in Housing Studies and a Bachelors degree in Social Sciences.
Contact:
Dr. Clare Xanthos
E-mail: clarexanthos@yahoo.com
Xanthos, Clare (2007). Conflicting Obligations: Role Conflict Among Health Care Complaints Managers [44 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 9(1), Art. 8, http://nbn-resolving.de/urn:nbn:de:0114-fqs080187.