

Volume 24, No. 2, Art. 18 – May 2023
Potentially Identifying Variables Reported in 100 Qualitative Health Research Articles: Implications for Data Sharing and Secondary Analysis
Annie B. Friedrich, Jessica Mozersky & James M. DuBois
Abstract: There is a growing trend in social science research to share qualitative data in a repository for others to access. However, some researchers are reticent to share qualitative data. One major concern is how to de-identify qualitative data while maintaining adequate contextual detail to allow secondary users to meaningfully interpret de-identified data. To help inform discussions regarding qualitative data sharing, we reviewed 100 qualitative health science studies to determine what potentially identifying variables (PIVs) are reported in the published literature. There are relatively few PIVs reported in each qualitative study; the majority of studies (n=64) reported two or fewer PIVs. The most commonly reported PIVs were profession, sex or gender, and age. Our findings can help guide de-identification efforts going forward as presumably the PIVs that are most commonly reported provide essential contextual details that will also be needed by secondary users, while PIVs that are rarely reported may not provide essential contextual information for interpretation of data. This suggests it is possible to share qualitative data that are both de-identified and useful for secondary analysis. As data are shared, we recommend researchers mask study sites, as these may uniquely increase the chance of re-identification.
Key words: qualitative data sharing; health sciences; secondary analysis; potentially identifying variables; de-identification
Table of Contents
1. Introduction
2. Methods
2.1 Article selection
2.2 Determining what potentially identifying variables are reported
2.3 Determining how potentially identifying variables are reported
2.4 Characterizing study site
3. Results
3.1 What potentially identifying variables are reported?
3.2 How are potentially identifying variables reported?
3.3 How many PIVs are reported in each study?
3.4 Characterizing study site(s)
4. Discussion
In some countries, such as the UK, Australia, and Germany, there has been a growing trend in social science research to share qualitative data in a repository for others to access (ALEXANDER et al., 2019; BISHOP & KUULA-LUUMI, 2017; CORTI, 2000; DuBOIS, STRAIT & WALSH, 2018; KARCHER, KIRILOVA, PAGÉ & WEBER, 2021; LEVENSTEIN & LYLE, 2018). This trend builds on the shift towards open science and the increasing requirements of funding institutions, professional associations, and journals to share and reuse data (ELMAN, KAPISZEWSKI & KIRILOVA, 2014; FELDMAN & SHAW, 2019; NOSEK et al., 2015; TAICHMAN et al., 2016). In the United States (US), quantitative data are frequently shared but the same is not true of qualitative data, which are rarely shared. In a recent survey of over 400 qualitative health researchers in the US, we found that 96% had never shared qualitative data in a repository (MOZERSKY et al., 2021). [1]
The National Institutes of Health (NIH), the largest federal funder of health research in the US, issued a new data sharing policy mandating data sharing as of 2023 regardless of whether data are qualitative or quantitative, including data that are not used in final publications (Notice Identification: NOT-OD-21-013). The policy requires all NIH funded investigators to submit data management and sharing plans to "integrate data sharing into the routine conduct of research" (NATIONAL INSTITUTES OF HEALTH, 2020, n.p.). Qualitative researchers who work in the health sciences, and are grant funded by the NIH, will need to be prepared to share data going forward to meet these new requirements. [2]
At the same time, researchers have expressed multiple concerns regarding qualitative data sharing (BROOM, CHESIRE & EMMISON, 2009; KIRILOVA & KARCHER, 2017; KUULA, 2011; MOZERSKY et al., 2021; MOZERSKY, WALSH et al., 2020; YARDLEY, WATTS, PEARSON & RICHARDSON, 2014). One of qualitative researchers' primary concerns is that the very process of de-identification would remove contextual details needed by secondary users to meaningfully analyze and interpret the data (BISHOP, 2009; HAMMERSLEY, 2010; MANNHEIMER, PIENTA, KIRILOVA, ELMAN & WUTICH, 2019; MOZERSKY, WALSH et al., 2020). These concerns are reflected in our survey of over 400 qualitative health researchers, where 79% of researchers reported concerns that data cannot be adequately de-identified and 74% said that data sharing would create the potential for misinterpretation of the data (MOZERSKY, WALSH et al., 2020). [3]
Qualitative data are often rich in detail and context not captured by quantitative methods, and frequently explore sensitive or stigmatized topics, especially in relation to health (BARBOUR, 2000; BROOM et al., 2009; DICKSON-SWIFT, JAMES, KIPPEN & LIAMPUTTONG, 2006; GUILLEMIN & HEGGEN, 2009). The ability to capture detailed, subtle, and often hidden aspects of people's experiences related to health is what makes qualitative methods a rich and important addition to quantitative data. However, the non-numeric nature of qualitative data also creates de-identification challenges. Removing standard variables such as names, addresses, or ID numbers may not suffice when data contain uniquely identifying information based on combinations of information such as job title, organization, and year (e.g., CEO of Google in 2006) or a sufficient combination of contextual details that may enable re-identification (e.g., a male, psychiatric nurse at local hospital X) to infer an identify (DuBOIS et al., 2018; KIRILOVA & KARCHER, 2017). [4]
However, we currently lack clear guidance on how to adequately de-identify qualitative data in a way that maintains confidentiality while leaving sufficient contextual detail to enable secondary use. In the US, the Health Insurance Portability and Accountability Act (HIPAA) provides a list of 18 "safe harbor" identifiers, including names, birth dates, medical record or device numbers, and phone numbers that must be removed for data to be considered de-identified. However, HIPAA requirements were designed for quantitative data found in the electronic medical record, and the majority of the 18 HIPAA safe harbor identifiers are unlikely to be present in qualitative data at all (GUPTA et al., 2021). HIPAA identifiers are specific to the US regulatory context and removing them helps to meet US regulatory de-identification requirements, but this alone is not sufficient for de-identifying qualitative data. Data repositories such as the UK Data Archive distinguish between direct and indirect identifiers (UK DATA SERVICE, 2023). Indirect identifiers—like a unique profession—present greater challenges when de-identifying qualitative data as they may be identifiable when combined with other data. Importantly, there are no agreed upon standards for determining when qualitative data can be considered de-identified or what variables must be removed to ensure data cannot be re-identified, or by whom (as it may always be that the interviewee and interviewer will be able to identify themselves). [5]
Qualitative data are much more likely to contain other types of variables that would not be considered HIPAA identifiers but that could potentially identify participants when combined with one another (McLELLAN, MacQUEEN & NEIDIG, 2016; TOLICH, 2004; TSAI et al., 2016). Throughout this paper, we refer to these as potentially identifying variables (PIV) because on its own a PIV will not identify a participant, but when multiple PIVs are combined, re-identification becomes more likely. [6]
In order to ethically and responsibly share qualitative data, researchers must balance the need to remove enough details to protect individual identities while leaving as much contextual details as possible to enable secondary users to interpret the data (MOZERSKY, WALSH et al., 2020). Data that are stripped of too many details may protect individual identities, but if the remaining data are rendered useless for secondary analyses because too many details have been removed, then the goals of data sharing cannot be met. [7]
For some qualitative researchers, the very notion of sharing data for others to use is problematic because, they argue, only the original investigators are capable of interpreting the data correctly due to their specific contextual knowledge of the data (FELDMAN & SHAW, 2019; KUULA, 2011; MOZERSKY, WALSH et al., 2020). In fact, some researchers only allow secondary use of their qualitative data when it will involve their direct collaboration with secondary researchers (FELDMAN & SHAW, 2019). From some methodological standpoints, researchers understand qualitative data as jointly constructed or "generated" by researcher and respondent in an iterative and intersubjective process that cannot be replicated by secondary users (BROOM et al., 2009, p.1164). [8]
Despite the concerns regarding secondary use, there are numerous benefits of qualitative data sharing such as enabling new research with existing data in cost-effective ways, collating existing data, training students in qualitative analysis with original data sets, and enhancing transparency in the research enterprise (ANTES, WALSH, STRAIT, HUDSON-VITALE & DuBOIS, 2018; BISHOP, 2009, 2014; CARUSI & JIROTKA, 2009; CHATFIELD, 2020; CORTI, 2007). Qualitative research participants may also support data sharing especially if it saves resources or avoids the need for recontact. We conducted qualitative interviews with 30 research participants who had taken part in sensitive qualitative health studies and found that the majority supported data sharing with other researchers so long as data were de-identified (MOZERSKY, PARSONS et al., 2020; VANDEVUSSE, MUELLER & KARCHER, 2022). Qualitative data sharing may also help mitigate study participant "research fatigue," or the psychological and emotional exhaustion that study participants, particularly those from small and/or marginalized communities, may experience when asked to participate in countless research projects. With increased qualitative data sharing, researchers can access important data sets without unduly burdening research participants (ASHLEY, 2020). At the same time, it is important to ensure that researchers do not become overly reliant on a single shared data set to avoid entrenchment. Realizing the benefits of data sharing requires overcoming the barriers and concerns of qualitative health researchers. [9]
In this paper, we set out to determine what potentially identifying variables (PIV) are reported by qualitative researchers in 100 qualitative health sciences articles that employed a focus group or interview methodology during a recent 12-month period. Given that a major barrier to sharing qualitative data is the claim that de-identification will remove too many contextual details and make secondary analyses unfeasible, we sought to examine what variables are actually reported in these articles. Our analysis is premised on the assumption that the variables reported by researchers in published literature are the essential contextual details needed for interpreting the data, and therefore provide the minimum adequate contextual details needed by secondary users. If a variable is not reported, then we assume it was not essential for interpretation of the data. Our analysis of these articles provides information on the number, types, and ways in which variables are commonly reported in qualitative health science research. This information can help inform future efforts to determine which identifiers are needed for interpretation by secondary users, and which can—in the view of authors—be shared without risking re-identification of participants. [10]
The data reported here were gathered as part of a larger NIH-funded project [RO1HG009351-04] to overcome barriers and facilitate ethical and responsible qualitative data sharing. This includes developing guidelines and software to support health science researchers in de-identifying qualitative data prior to sharing with a repository where others can access them for secondary use (DuBOIS et al., 2018). In our project, we analyzed data from interviews or focus groups—primarily transcripts from recorded conversations. We do not currently intend to share other forms of qualitative data such as field notes or visual data such as photographs, as these present greater challenges for de-identification. [11]
We begin with a description of our methods, including how we determined what could be considered a potentially identifying variable (Section 2). We report the results of our analysis in Section 3 and discuss implications for data sharing and secondary analysis in Section 4. [12]
To collect a broad sample of qualitative health science research involving interviews or focus groups, we searched PubMed for articles published between November 1, 2019 and October 31, 2020 using the search terms: "qualitative AND ("interview" OR "focus group"). We randomly selected 50 articles that met our inclusion criteria (human subjects research, published in English, indexed in MEDLINE, using an interview or focus group methodology). We also randomly selected 50 qualitative health science research articles from top-ranked health science journals as indicated by impact factor. This strategy ensured that we captured a wide variety of qualitative health science articles that could serve to represent the field. Our full search strategy for collecting a representative sample of qualitative health science research has been described elsewhere (MOZERSKY, FRIEDRICH & DuBOIS, 2022).1) [13]
2.2 Determining what potentially identifying variables are reported
All authors were involved in initial codebook development, which was originally developed as part of our larger project to determine what non-HIPAA identifiers were likely to be present in qualitative data. These data informed the development of software we are creating that assists with de-identification of qualitative data (GUPTA et al., 2021). Our codebook contained the 18 HIPAA identifiers, and a list of other potentially identifying variables that may be reported in qualitative health science research (ibid.) (see Table 1). We allowed for inductive coding if we found any PIVs during coding that we did not anticipate and that were not contained in our original codebook. [14]
We differentiate between PIVs that are inclusion criteria and apply to the entire sample (e.g., nurses, students) from those PIVs that are connected to a specific participant quote (e.g., 35-year-old female). Both could potentially be identifying of an individual participant, but this will almost always be due to a combination of PIVs, rather than a single PIV. [15]
2.3 Determining how potentially identifying variables are reported
We also coded for any indication that researchers attempted to mask a particular PIV to protect participant privacy. We created a "masking" code which was defined as any attempt to present data more broadly or mask an inclusion or individual identifier, including generalization (e.g., health center in an urban area), obvious redaction, using study ID numbers to identify participants, or using pseudonyms. [16]
We also coded each article for whether the research was carried out at a single site or institution, multiple sites or institutions, or more broadly within a particular community or group of participants. We included study site because knowing the site may increase the chances that an individual could be re-identified when combined with other PIVs, especially if it is the only site where research was conducted. We distinguished study site from an organization or institution by defining study site as the location where the specific study took place, whereas an organization or institution could be mentioned anywhere in the data but did not necessarily refer to the specific site where the research was conducted. [17]
During the first phase of coding, two coders (AF and JM) blind coded two articles, discussed and resolved differences in coding, and made changes to the codebook. The coders repeated this process until codes were consistently applied to the articles without major discrepancies between the raters. The primary coder (AF) proceeded to code half of the articles, at which point another blind coding check was conducted with the second coder (JM) to ensure ongoing agreement and consistent application of codes. Coders resolved differences in coding during consensus meetings and revised the codebook accordingly.
Table 1: Categories of potentially identifying variables reported in the sample of articles. Click here to download the PDF file. [18]
3.1 What potentially identifying variables are reported?
We first assessed which PIVs were reported in the articles and whether these characteristics applied to all study participants (inclusion PIV) or were used to provide key contextual or individual participant characteristics immediately following a participant quote (individual PIV) (Table 2). Given the unique nature of study site as a potentially identifying variable, we analyzed this PIV separately (see Table 5). [19]
The most commonly reported PIV was profession (reported in 64 articles); in over half of these instances (36 articles) profession was an inclusion criterion (e.g., a study of nurses or residents). The remaining 28 articles reported profession in relation to individual participants following a quote, and this was masked in 16 articles. Sex or gender (45 articles) and age (23 articles) were the next most commonly reported PIVs (Table 2). Sex or gender was never masked and was most often reported as an individual PIV following a quote. Age was never an inclusion PIV, and very rarely masked as an age range (3 out of 23 studies). The remaining PIVs—institution or organization names (not related to study site), race, ethnicity, indigenous status or nationality, marital status, education level, and rare disease or illness—were rarely reported, and we saw no instances of LGBTQI or foreign language or dialect PIVs. [20]
Of the three most commonly occurring PIVs (profession, sex/gender, and age), age and sex/gender are reported together in 14 articles, profession and sex/gender are reported together in 21 articles, and age and profession are reported together in 22 articles. Only 14 articles report all three of the most commonly occurring PIVs in combination.
Table 2: Number of articles containing potentially identifying variables. Click here to download the PDF file. [21]
3.2 How are potentially identifying variables reported?
We also assessed whether researchers attempted to mask a particular PIV to protect participant privacy. Eighty-six articles utilized at least one masking strategy, and the most common masking practice was generalization, with almost 70% of articles employing this masking strategy for an inclusion PIV, individual PIV, or study site. Assigning a participant ID was another common masking strategy. Using a pseudonym or fully redacting information were rarely utilized (Table 3).
Table 3. Masking characteristics. Click here to download the PDF file. [22]
3.3 How many PIVs are reported in each study?
We calculated how many PIVs were reported within each article, distinguishing between inclusion PIVs and individual PIVs. In forty articles, researchers reported no individual PIVs (Table 4). In the majority of articles (64), researchers reported 2 or fewer PIVs of any kind (either inclusion or individual PIVs) (Figure 1).
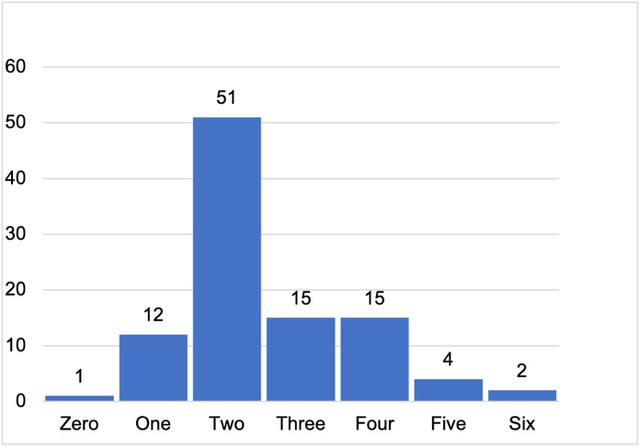
Figure 1: Percent of articles with zero to six PIVs (inclusion + individual)
Table 4: Number of inclusion and individual PIV categories reported per article. Click here to download the PDF file. [23]
3.4 Characterizing study site(s)
Because knowing an individual study site could be highly identifying for participants in certain contexts, especially in combination with other reported PIVs, we analyzed whether the study was conducted at a single site or institution, multiple sites or institutions, or conducted more broadly within a community. We also assessed whether any masking strategies were employed. Thirty-two studies were conducted at a single site, and 13 of these studies named the specific institution where research was conducted. Twenty-two studies were conducted at multiple sites, and only 1 study named the specific participating institutions. Forty-six studies were conducted within broader communities or with a generalized group of participants, rather than a particular site or institution. Generalized or broad community research may be masked by the nature of the research (i.e., there is no particular institution or organization to pseudonymize or generalize) (Table 5). We also assessed whether any HIPAA geographic locations (geographic subdivisions smaller than a state) were reported. In thirty-nine studies, researchers included a HIPAA geographic location to further describe study site. We found 4 articles describing broad community research in which participants were individually identified as belonging to one of the specific communities where the research was conducted, potentially increasing their identifiability.
Table 5: Type of study site. Click here to download the PDF file. [24]
One main argument against qualitative data sharing is that de-identification to adequately protect participant anonymity will remove important contextual details needed for accurate secondary interpretation of the data (BROOM et al., 2009; FELDMAN & SHAW, 2019). In light of the increasing trends and requirements for qualitative data sharing, we sought to determine what potentially identifying variables (PIVs) are reported in a representative sample of qualitative health science literature. This information can help guide de-identification efforts going forward by providing a better understanding of which PIVs are most commonly reported and presumably considered to be essential contextual details needed by secondary users, and which PIVs are rarely reported and presumably not viewed as essential contextual information for interpretation of data. To our knowledge, this is the first study to seek this information. [25]
Our findings show that there are relatively few PIVs reported in individual published qualitative health science research studies; most variables we anticipated finding based on our codebook are not commonly reported by qualitative researchers. We found no instances of the 18 HIPAA safe harbor identifiers apart from cities describing study site, which is unsurprising since most identifiers were designed with quantitative data in mind (GUPTA et al., 2021). More notably, the majority of non-HIPAA PIV categories in our codebook were also rarely, or never, reported (i.e., race or ethnicity, education, rare diseases, LGBTQI status). The most commonly reported PIVs were profession, sex or gender, and age. All three of the most commonly occurring PIVs were reported together in only 14 articles. Because PIVs or study sites may be masked, these combinations likely provide important contextual information while maintaining a low risk of participant re-identification. This suggests that authors likely can report age, sex/gender, and profession—alone or in combination—to further contextualize their data. [26]
In the majority of studies (n=64), researchers reported two or fewer PIV categories, and in nearly half of the studies (n=40), researchers reported no individual PIVs following a participant quote at all. In these cases, the only PIVs were inclusion criteria that applied to all participants (i.e., females, physicians, etc.). This suggests that many variables could be removed from data for the purpose of de-identification while leaving the most essential variables for context and interpretation in the data. Of course, when such information will not enable inferential re-identification of participants, it may be safely left, which would provide secondary users with more natural and complete text and associated context. [27]
We also analyzed study site information because knowing the study site may increase the chances that an individual could be re-identified when combined with other PIVs. The majority of studies (n=68) were conducted at multiple sites or were generalized to broad communities or participant groups, which reduces the chance of re-identification based on a specific location. However, we did find a small number of generalized and broad community articles in which researchers individually identified participants as belonging to one of the specific communities or cities where the research was conducted, potentially increasing their identifiability. Thirty-two studies took place at a single study site, 13 of which named specific institutions. These single-site studies may pose the greatest risk of reidentification of participants when combined with other PIVs, particularly individual PIVs attached to participant quotes. For example, the following participant quote was published in a study that took place at the University of California San Francisco (UCSF):
"[The patient] said 'I looked at your name and thought I would see someone that looks more like me. I don't want to talk to you.' And she started yelling at us to leave. Then the attending came in and she started yelling at him too because he was black. [Fourth-year medical student, woman, Latina]" (WHEELER et al., 2019, p.1680). [28]
Because we know the participant is a female of Hispanic descent (referred to as "Latina" by the authors) and a fourth-year medical student at a particular institution (UCSF), colleagues may potentially be more able to re-identify her. However, because UCSF is a large institution with many Hispanic students, study authors likely felt that the risk was low. In contrast, it is much harder to identify participants in multi-site studies or when participants are drawn from a broader region or country who meet study criteria (TSAI et al., 2016). Using the example quote above, if the study was conducted at 3 academic medical centers, the chances that this individual could be re-identified in combination with other PIVs is greatly reduced. Researchers will need to weigh the risks associated with conducting their study at a single site and take steps to mitigate those risks, such as appropriate masking or generalization to include meaningful context about their site while also protecting participants. Researchers will also need further education, given that 13 out of 23 single site studies did not mask the site, while the majority of multi-site studies were masked or generalized in some way (21 out of 22 studies). [29]
Our overall findings suggest that published data do not include many potentially identifying contextual details. Little violence would be done to shared data by masking some PIVs; and some PIVs (profession, age, and sex/gender) can, it appears from these 100 studies, be safely shared unmasked without a significant risk of identifying participants. At the same time, many questions remain about how to conduct responsible and ethical secondary analysis of qualitative health science research. Currently, de-identification of qualitative data is primarily done manually with researchers removing what they deem to be necessary based on the context, and we lack guidelines and standards for how to safely and ethically de-identifying qualitative data (KIRILOVA & KARCHER, 2017). Given the nature of qualitative research, there may be no definitive combination or number of identifiers that pose a particular risk to participant privacy, so individual researchers will need to assess each study individually to determine what PIVs should be removed. We found that participants are supportive of sharing their qualitative data so long as it is de-identified, but questions remain about when qualitative data can be considered adequately de-identified, which requires balancing removing identifying information while leaving enough contextual detail to enable secondary use (MOZERSKY, PARSONS et al., 2020). Study participants should also be given the opportunity to share their perspectives on what information they consider identifying, which is an area for future research. [30]
We also lack guidelines on appropriate secondary use, which is an important area for future research (KIRILOVA & KARCHER, 2017; YOON, 2014). Data repositories and curators with experience with qualitative data can work with researchers to ensure that they provide appropriate context for the data and document what the data do not contain—to help secondary users assess how the information available to them differs from that available to the original researchers, and help convey the researchers' original epistemological or theoretical commitments (KARCHER et al., 2021). While some critics argue that it is not possible to reuse archived data without access to the original context in which it was produced, others argue that "recontextualizing data" opens up new possibilities for data reuse and theory building (BISHOP, 2006; MOORE, 2006). In fact, researchers' intimate knowledge of the original research context can be a boon to sharing, as they are well positioned to make necessary modifications to data without harming participants or the data themselves (KIRILOVA & KARCHER, 2017). [31]
Researchers can also choose to make their qualitative data only available via restricted access, which requires that secondary users have the appropriate approvals prior to accessing the data. Whenever qualitative data is archived for reuse, sharing and reanalysis should be carried out in ways that fit the particular research tradition (KAPISZEWSKI & KIRILOVA, 2014; LUPIA & ELMAN, 2013). Some data collection methods such as ethnography with extensive personal field notes may create greater challenges for de-identification prior to sharing. Researchers, data curators, and academic librarians can work together to find the balance between sharing as much as possible without introducing undue additional risk (KIRILOVA & KARCHER, 2017). Restricted access is likely the most appropriate way to share qualitative data given the lack of guidance regarding de-identification and secondary analyses currently. Regardless of how qualitative data are shared, it is essential that researchers obtain permission for data sharing from the research participants themselves. Consent forms must convey information regarding data sharing in a way that is understandable and acceptable to participants. [32]
Our study has several important limitations. First, we focused only on qualitative health science research, which does not represent the breadth and diversity of contexts where qualitative research is conducted. Similarly, our focus on studies involving interviews and focus groups cannot be generalized to other methods such as participant observation or oral histories. In fact, oral histories involve making participant names public; de-identification concerns are unlikely to be relevant for oral histories, while field notes from participant observation may be especially challenging to de-identify and may not be suitable for sharing. Yet even with these limitations, our findings contribute to important ongoing debates and discussion about secondary use and suggest that qualitative health science researchers may be able to share interview and focus group data much more readily than critics claim. [33]
Abdi, Batula; Okal, Jerry; Serour, Gamal & Temmerman, Marleen (2020). "Children are a blessing from God"—A qualitative study exploring the socio-cultural factors influencing contraceptive use in two Muslim communities in Kenya. Reproductive Health, 17(1), 44, https://doi.org/10.1186/s12978-020-0898-z [Accessed: October 1, 2022].
Agarwal, Sumit D.; Pabo, Erika; Rozenblum, Ronen & Sherritt, Karen M. (2020). Professional dissonance and burnout in primary care: A qualitative study. JAMA Internal Medicine, 180(3), 395-401.
Ahmad, Fayaz; Boeckmann, Melanie; Khan, Zohaib; Zeeb, Hajo; Khan, Muhammad Naseem; Ullah, Safat; Dreger, Steffen; Ul Haq, Zia & Forberger, Sarah (2020). Implementing smokeless tobacco control policy in Pakistan: A qualitative study among Naswar supply chain actors. Tobacco Control, 30(5), 548-552, https://doi.org/10.1136/tobaccocontrol-2020-055748 [Accessed: October 1, 2022].
Ahonsi, Babatunde; Fuseini, Kamil; Nai, Dela; Goldson, Erika; Owusu, Selina; Ndifuna, Ismail; Humes, Icilda & Tapsoba, Placide L. (2019). Child marriage in Ghana: Evidence from a multi-method study. BMC Womens Health, 19(1), 126, https://doi.org/10.1186/s12905-019-0823-1 [Accessed: October 1, 2022].
Aloweni, Fazila; Doshi, Kinjal; Fook-Chong, Stephanie; Malhotra, Rahul & Østbye, Truls (2019). The types of caregiving reactions experienced by the older spouse caregivers. Journal of Clinical Nursing, 28(23-24), 4538-4548.
Alpren, Charles; Dawson, Erica L.; John, Betsey; Cranston, Kevin; Panneer, Nivedha; Fukuda, H. Dawn; Roosevelt, Kathleen; Klevens, R. Monica; Bryant, Janice; Peters, Phillip J.; Lyss, Sheryl B.; Switzer, William M.; Burrage, Amanda; Murray, Ashley; Agnew-Brune, Christine; Stiles, Tracy; McClung, Paul; Campbell, Ellsworth M.; Breen, Courtney; Randall, Liisa M.; Dasgupta, Sharoda; Onofrey, Shauna; Bixler, Danae; Hampton, Kischa; Jaeger, Jenifer Leaf; Hsu, Katherine K.; Adih, William; Callis, Barry; Goldman, Linda R.; Danner, Susie P.; Jia, Hongwei; Tumpney, Matthew; Board, Amy; Brown, Catherine; DeMaria, Jr., Alfred & Buchacz, Kate (2020). Opioid use fueling HIV transmission in an urban setting: An outbreak of HIV infection among people who inject drugs-Massachusetts, 2015-2018. American Journal of Public Health, 110(1), 37-44.
Andrade, Lesley; Moran, Kathy; Snelling, Susan J.; Malaviarachchi, Darshaka; Beyers, Joanne; Near, Kelsie & Randall Simpson, Janis (2020). Beyond BMI: A feasibility study implementing NutriSTEP in primary care practices using electronic medical records (EMRs). Health Promotion and Chronic Disease Prevention in Canada, 40(1), 1-10.
Armstrong, Stephanie; Langlois, Adele; Siriwardena, Niroshan & Quinn, Tom (2019). Ethical considerations in prehospital ambulance based research: Qualitative interview study of expert informants. BMC Medical Ethics, 20(1), 88, https://doi.org/10.1186/s12910-019-0425-3 [Accessed: October 1, 2022].
Bagherian, Samaneh; Sharif, Farkhondeh; Zarshenas, Ladan; Torabizadeh, Camellia; Abbaszadeh, Abbas & Izadpanahi, Payam (2020). Cancer patients' perspectives on dignity in care. Nursing Ethics, 27(1), 127-140.
Baker, John A.; Canvin, Krysia & Berzins, Kathryn (2019). The relationship between workforce characteristics and perception of quality of care in mental health: A qualitative study. International Journal of Nursing Studies, 100, 103412.
Banke-Thomas, Aduragbemi; Maua, Judith; Madaj, Barbara; Ameh, Charles & van den Broek, Nynke (2020). Perspectives of stakeholders on emergency obstetric care training in Kenya: A qualitative study. International Health, 12(1), 11-18, https://doi.org/10.1093/inthealth/ihz007 [Accessed: October 1, 2022].
Barnert, Elizabeth S.; Lopez, Nathalie & Chung, Paul J. (2020). Barriers to health care for Latino youths during community reentry after incarceration: Los Angeles County, California, 2016-2018. American Journal of Public Health, 110(S1), S63-S70, https://doi.org/10.2105/ajph.2019.305374 [Accessed: October 1, 2022].
Besigye, Innocent K.; Onyango, Jude; Ndoboli, Fred; Hunt, Vincent; Haq, Cynthia & Namatovu, Jane (2019). Roles and challenges of family physicians in Uganda: A qualitative study. African Journal of Primary Health Care & Family Medicine, 11(1), e1-e9, https://doi.org/10.4102/phcfm.v11i1.2009 [Accessed: October 1, 2022].
Binka, Charity; Nyarko, Samuel H.; Awusabo-Asare, Kofi & Doku, David T. (2019). Barriers to the uptake of cervical cancer screening and treatment among rural women in Ghana. Biomed Research International, https://doi.org/10.1155/2019/6320938 [Accessed: October 1, 2022].
Blank, Mei-Ling; Hoek, Janet & Gendall, Philip (2021). Roll-your-own smokers' reactions to cessation-efficacy messaging integrated into tobacco packaging design: A sequential mixed-methods study. Tobacco Control, 30(4), 405-412.
Bowen, Judith L.; Ilgen, Jonathan S.; Regehr, Glenn; Cate, Olle ten; Irby, David M. & O'Brien, Bridget C. (2019). Reflections from the rearview mirror: Internal medicine physicians' reactions to clinical feedback after transitions of responsibility. Academic Medicine, 94(12), 1953-1960, https://doi.org/10.1097/acm.0000000000002831 [Accessed: October 1, 2022].
Brown, Jennifer; Zhu, Meng; Moran, Meghan; Hoe, Connie; Frejas, Ferdie & Cohen, Joanna E. (2021). "It has candy. You need to press on it": Young adults' perceptions of flavoured cigarettes in the Philippines. Tobacco Control, 30(3), 293-298, https://doi.org/10.1136/tobaccocontrol-2019-055524 [Accessed: October 1, 2022].
Burbridge, Claire; Randall, Jason A.; Lawson, Joe; Symonds, Tara; Dearden, Lindsay; Lopez-Gitlitz, Angela; Espina, Byron & McQuarrie, Kelly (2020). Understanding symptomatic experience, impact, and emotional response in recently diagnosed metastatic castration-resistant prostate cancer: A qualitative study. Supportive Care in Cancer, 28(7), 3093-3101.
Byhoff, Elena & Taylor, Lauren A. (2019). Massachusetts community-based organization perspectives on medicaid redesign. American Journal of Preventive Medicine, 57(6 Suppl 1), S74-S81, https://doi.org/10.1016/j.amepre.2019.07.017 [Accessed: October 1, 2022].
Byhoff, Elena; De Marchis, Emilia H.; Hessler, Danielle; Fichtenberg, Caroline; Adler, Nancy; Cohen, Alicia J.; Doran, Kelly M.; de Cuba, S Stephanie Ettinger; Fleeger, Eric W.; Gavin, Nicholas; Huebschmann, Amy G.; Tessler Lindau, Stacy; Tung, Elizabeth L.; Raven, Maria; Jepson, Susan; Johnson, Wendy; Olson, Ardis L.; Sandel, Megan & Gottlieb, Laura M. (2019). Part II: A qualitative study of social risk screening acceptability in patients and caregivers. American Journal of Preventive Medicine, 57(6 Suppl 1), S38-s46, https://doi.org/10.1016/j.amepre.2019.07.016 [Accessed: October 1, 2022].
Chavez, Gladis; Minkler, Meredith; McDaniel, Patricia A., Estrada, Jessica; Thayer, Ryan & Falbe, Jennifer (2019). Retailers' perspectives on selling tobacco in a low-income San Francisco neighbourhood after California's $2 tobacco tax increase. Tobacco Control, 28(6), 657-662.
Chukwuma, Adanna; Gong, Estelle; Latypova, Mutriba & Fraser-Hurt, Nicole (2019). Challenges and opportunities in the continuity of care for hypertension: A mixed-methods study embedded in primary health care intervention in Tajikistan. BMC Health Services Research, 19, 925, https://doi.org/10.1186/s12913-019-4779-5 [Accessed: October 1, 2022].
Crape, Byron L.; Yakhiyayeva, Tansholpan; Kadyrzhanuly, Kainar; Gusmanov, Arnur & Sadykova, Dzhamilya (2020). Hookah venue employees' knowledge and perceptions of hookah tobacco smoking. Tobacco Control, 30(3), 299-304.
Davies, A.R.; Homolova, L.; Grey, C.N.B. & Bellis, M.A. (2019). Health and mass unemployment events-developing a framework for preparedness and response. Journal of Public Health (Oxf), 41(4), 665-673, https://doi.org/10.1093/pubmed/fdy174 [Accessed: October 1, 2022].
De Carvalho, Mariana Lustosa; Barbosa, Cristhiano Neiva Santos; Bezerra, Valéria Peixoto; dos Santos, Ana Maria Ribeiro; Silva, Cynthia Roberta Dias Torres; de Brito, Cleidiane Maria Sales & Figueiredo, Maria do Livramento Fortes (2019). Health situation in the perception of elderly widows assisted by primary health care. Revista Brasileira de Enfermagem, 72(Suppl 2), 199-204, https://doi.org/10.1590/0034-7167-2018-0549 [Accessed: October 1, 2022].
De Oliveira, Valéria Conceição; Guimarães, Eliete Albano de Azevedo; Amaral, Gabriela Gonçalves; Silva, Talita Ingrid Magalhães; Fabriz, Luciana Aparecida & Pinto, Ione Carvalho (2020). Acceptance and use of the Information System of the National Immunization Program. Revista Latin America Enfermagem, 28, e3307, https://doi.org/10.1590/1518-8345.3360.3307 [Accessed: October 1, 2022].
Devik, Siri Andreassen; Enmarker, Ingela & Hellzen, Ove (2020). Nurses' experiences of compassion when giving palliative care at home. Nursing Ethics, 27(1), 194-205.
Dogan, Elizabeth Irene Karlsen; Raustøl, Anne & Terragni, Laura (2020). Student nurses' views of right to food of older adults in care homes. Nursing Ethics, 27(3), 754-766.
Doubleday, Annie; Errett, Nicole A.; Ebi, Kristie L. & Hess, Jeremy J. (2020). Indicators to guide and monitor climate change adaptation in the US Pacific Northwest. American Journal of Public Health, 110(2), 180-188, https://doi.org/10.2105/ajph.2019.305403 [Accessed: October 1, 2022].
Enoch, Abigail J.; English, Mike; the Clinical Information Network; McGivern, Gerald & Shepperd, Sasha (2019). Variability in the use of pulse oximeters with children in Kenyan hospitals: A mixed-methods analysis. PLoS Medicine, 16(12), e1002987, https://doi.org/10.1371/journal.pmed.1002987 [Accessed: October 1, 2022].
Feller, Katrin & Berendonk, Christopher (2020). Identity matters—perceptions of inter-professional feedback in the context of workplace-based assessment in diabetology training: A qualitative study. BMC Medical Education, 20(1), 33, https://doi.org/10.1186/s12909-020-1932-0 [Accessed: October 1, 2022].
Fernandes, Hugo; Brandão, Maykon Brito; de Castilho-Júnior, Roberto Alvarenga; Hino, Paula & Ohara, Conceição Vieira da Silva (2020). The care for the persistent family aggressor in the perception of nursing students. Revista Latin America Enfermagem, 28, e3287, https://doi.org/10.1590/1518-8345.3991.3287 [Accessed: October 1, 2022].
Fulford, Hamish; McSwiggan, Linda; Kroll, Thilo & MacGillivray, Stephen (2019). Exploring the use of mobile information and communication technologies by people with mood disorders. International Journal of Mental Health Nursing, 28(6), 1268-1277.
Gysin, Stefan; Sottas, Beat; Odermatt, Muriel & Essig, Stefan (2019). Advanced practice nurses' and general practitioners' first experiences with introducing the advanced practice nurse role to Swiss primary care: A qualitative study. BMC Family Practice, 20(1), 163, https://doi.org/10.1186/s12875-019-1055-z [Accessed: October 1, 2022].
Haggart, Kerri; Robertson, Lindsay; Blank, Mei-Ling; Popova, Lucy & Hoek, Janet (2020). It's just steam: A qualitative analysis of New Zealand ENDS users' perceptions of secondhand aerosol. Tobacco Control, 30(1), 30-35, https://doi.org/10.1136/tobaccocontrol-2019-055368 [Accessed: October 1, 2022].
Honkavuo, Leena (2020). Nursing students' perspective on a caring relationship in clinical supervision. Nursing Ethics, 27(5), 1225-1237.
Huber-Krum, Sarah; Hackett, Kristy; Senderowicz, Leigh; Pearson, Erin; Francis, Joel M.; Siril, Hellen; Ulenga, Nzovu & Shah, Iqbal (2019). Women's perspectives on postpartum intrauterine devices in Tanzania. Studies in Family Planning, 50(4), 317-336, https://doi.org/10.1111/sifp.12106 [Accessed: October 1, 2022].
Hunter, Kiri & Cook, Catherine (2020). Indigenous nurses' practice realities of cultural safety and socioethical nursing. Nursing Ethics, 27(6), 1472-1483.
Isler, Jasmin; Sawadogo, N. Hélène; Harling, Guy; Bärnighausen, Till; Adam, Maya; Kagoné, Moubassira; Sié, Ali; Greuel, Merlin & McMahon, Shannon A. (2019). Iterative adaptation of a mobile nutrition video-based intervention across countries using human-centered design: Qualitative study. Journal of Medical Internet Research, 7(11), e13604, https://doi.org/10.2196/13604 [Accessed: October 1, 2022].
Janssen, Ricky; Engel, Nora; Esmail, Aliasgar; Oelofse, Suzette; Krumeich, Anja; Dheda, Keertan & Pai, Nitika Pant (2020). Alone but supported: A qualitative study of an HIV self-testing app in an observational cohort study in South Africa. AIDS and Behavior, 24(2), 467-474, https://doi.org/10.1007/s10461-019-02516-6 [Accessed: October 1, 2022].
Jensen, Anders Møller; Pedersen, Birthe D.; Wilson, Rhonda L.; Bang Olsen, Rolf & Hounsgaard, Lise (2019). Nurses' experiences of delivering acute orthopaedic care to patients with dementia. International Journal of Older People Nursing, 14(4), e12271.
Kerrigan, Deanna; Sanchez Karver, Tahilin; Muraleetharan, Ohvia; Savage, Virginia; Mbwambo, Jessie; Donastorg, Yeycy; Likindikoki, Samuel; Perez, Martha; Gomez, Holsex; Mantsios, Andrea; Murray, Miranda; Beckham, S. Wilson; Davis, Wendy; Galai, Noya & Barrington, Clare (2020). "A dream come true": Perspectives on long-acting injectable antiretroviral therapy among female sex workers living with HIV from the Dominican Republic and Tanzania. PLoS One, 15(6), e0234666, https://doi.org/10.1371/journal.pone.0234666 [Accessed: October 1, 2022].
Kielo, Emilia; Suhonen, Riitta; Salminen, Leena & Stolt, Minna (2019). Competence areas for registered nurses and podiatrists in chronic wound care, and their role in wound care practice. Journal of Clinical Nursing, 28(21-22), 4021-4034.
Krupic, Ferid (2020). The impact of religion and provision of information on increasing knowledge and changing attitudes to organ donation: An intervention study. Journal of Religion and Health, 59(4), 2082-2095, https://doi.org/10.1007/s10943-019-00961-0 [Accessed: October 1, 2022].
Lai, Hui-Ling; Perng, Shoa-Jen & Huang, Chiung-Yu (2019). Nursing students' perceptions of a silent mentor program in an anatomy course. Anatomical Sciences Education, 12(6), 627-635.
Lalla, Amber Trujillo; Ginsbach, Katherine Farrell; Penney, Naomi; Shamsudin, Arsity & Oka, Rahul (2020). Exploring sources of insecurity for Ethiopian Oromo and Somali women who have given birth in Kakuma Refugee Camp: A qualitative study. PLoS Medicine, 17(3), e1003066, https://doi.org/10.1371/journal.pmed.1003066 [Accessed: October 1, 2022].
Li, Anyie J.; Tabu, Collins; Shendale, Stephanie; Okoth, Peter O.; Sergon, Kibet; Maree, Ephantus; Mugoya, Isaac K.; Machekanyanga, Zorodzai; Onuekwusi, Iheoma U. & Ogbuanu, Ikechukwu Udo (2020). Qualitative insights into reasons for missed opportunities for vaccination in Kenyan health facilities. PLoS One, 15(3), e0230783, https://doi.org/10.1371/journal.pone.0230783 [Accessed: October 1, 2022].
Li, Huanhuan; Sun, Dan; Wan, Zhenzhen; Chen, Jialu & Sun, J. (2020). The perceptions of older nurses regarding continuing to work in a nursing career after retirement: A qualitative study in two Chinese hospitals of different levels. International Journal of Nursing Studies, 105, 103554.
Lusambili, Adelaide M.; Naanyu, Violet; Wade, Terrance J.; Mossman, Lindsay; Mantel, Michaela; Pell, Rachel; Ngetich, Angela; Mulama, Kennedy; Nyaga, Lucy; Obure, Jerim & Temmerman, Merleen (2020). Deliver on your own: Disrespectful maternity care in rural Kenya. PLoS One, 15(1), e0214836, https://doi.org/10.1371/journal.pone.0214836 [Accessed: October 1, 2022].
Malâtre-Lansac, Angele; Engel, Charles C.; Xenakis, Lea; Carlasare, Lindseyy; Blake, Kathleen; Vargo, Carol; Botts, Christopher Chen, Peggy G. & Friedberg, Mark W. (2020). Factors influencing physician practices' adoption of behavioral health integration in the United States: A qualitative study. Annals of Internal Medicine, 173(2), 92-99.
Martinsen, Elin Håkonsen; Weimand, Bente & Norvoll, Reidun (2020). Does coercion matter? Supporting young next-of-kin in mental health care. Nursing Ethics, 27(5), 1270-1281.
McGuinness, Sarah L.; O'Toole, Joanne; Ayton, Darshini; Giriyan, Asha; Gaonkar, Chetan A.; Vhaval, Ramkrishna; Cheng, Allen C. & Leder, Karin (2020). Barriers and enablers to intervention uptake and health reporting in a water intervention trial in rural India: A qualitative explanatory study. American Journal of Tropical Medicine and Hygiene, 102(3), 507-517, https://doi.org/10.4269/ajtmh.19-0486 [Accessed: October 1, 2022].
McLeod, Katherine E. & Norman, Kathleen E. (2020). "I've found it's very meaningful work": Perspectives of physiotherapists providing palliative care in Ontario. Physiotherapy Research International, 25(1), e1802.
Melody, Shannon M., Martin-Gall, Veronica A. & Veitch, Mark G. (2021). Why Tasmanian retailers stop selling tobacco and implications for tobacco control. Tobacco Control, 30(5), 583-586.
Mishra, Divya; Spiegel, Paul B.; Digidiki, Vasileia Lucero & Winch, Peter J. (2020). Interpretation of vulnerability and cumulative disadvantage among unaccompanied adolescent migrants in Greece: A qualitative study. PloS Medicine, 17(3), e1003087, https://doi.org/10.1371/journal.pmed.1003087 [Accessed: October 1, 2022].
Moukarzel, Sara; Mamas, Christoforos; Farhat, Antoin; Abi Abboud, Antoine & Daly, Alan J. (2020). A qualitative examination of barriers against effective medical education and practices related to breastfeeding promotion and support in Lebanon. Medical Education Online, 25(1), 1723950, https://doi.org/10.1080/10872981.2020.1723950 [Accessed: October 1, 2022].
Nassery, Wazhma & Landgren, Kajsa (2019). Parents' experience of their sleep and rest when admitted to hospital with their ill child: A qualitative study. Comprehensive Child and Adolescent Nursing, 42(4), 265-279, https://doi.org/10.1080/24694193.2018.1528310 [Accessed: October 1, 2022].
Ng, P.Y., Lau, S.T., Ong, S. F. & Liaw, S.Y. (2019). Singaporean nursing students' perceptions of a career in community nursing. International Nursing Review, 66(4), 514-522.
Ohayon, Jennifer Liss; Nost, Eric; Silk, Kami; Rakoff, Michele & Brody, Julia Green (2020). Barriers and opportunities for breast cancer organizations to focus on environmental health and disease prevention: a mixed-methods approach using website analyses, interviews, and focus groups. Environmental Health, 19(1), 15, https://doi.org/10.1186/s12940-020-0570-7 [Accessed: October 1, 2022].
Østengaard, Lasse; Lundh, Andreas; Tjørnhøj-Thomsen, Tine; Abdi, Suhayb; Gelle, Mustafe H. A.; Stewart, Lesley A.; Boutron, Isabelle & Hróbjartsson, Asbjørn (2020). Influence and management of conflicts of interest in randomised clinical trials: Qualitative interview study. BMJ, 371, m3764, https://doi.org/10.1136/bmj.m3764 [Accessed: October 1, 2022].
Palamar, Joseph J; Acosta, Patricia; Sutherland, Rachel; Shedlin, Michele G. & Barratt, Monica J. (2019). Adulterants and altruism: A qualitative investigation of "drug checkers" in North America. International Journal of Drug Policy, 74, 160-169.
Parker, Lisa; Fabbri, Alice; Grundy, Quinn; Mintzes, Barbara & Bero, Lisa (2019). "Asset exchange"-interactions between patient groups and pharmaceutical industry: Australian qualitative study. BMJ, 367, l6694, https://doi.org/10.1136/bmj.l6694 [Accessed: October 1, 2022].
Pearce, Susie; Whelan, Jeremy; Kelly, Daniel M. & Gibson, Faith (2020). Renegotiation of identity in young adults with cancer: A longitudinal narrative study. International Journal of Nursing Studies, 102, 103465.
Qvist, Ninni; Bergström, Ingrid; Åkerstedt, Torbjörn; Persson, Jan; Konradsen, Hanne & Forss, Anette (2019). From being restrained to recapturing vitality: Non-western immigrant women's experiences of undergoing vitamin D treatment after childbirth. International Journal of Qualitative Studies on Health and Well-Being, 14(1), 1632111, https://doi.org/10.1080/17482631.2019.1632111 [Accessed: October 1, 2022].
Rashid, Abdul; Iguchi, Yufu & Afiqah, Siti Nur (2020). Medicalization of female genital cutting in Malaysia: A mixed methods study. PLoS Medicine, 17(10), e1003303, https://doi.org/10.1371/journal.pmed.1003303 [Accessed: October 1, 2022].
Ray-Barruel, Gillian; Woods, Christine; Larsen, Emily N.; Marsh, Nicole; Ullman, Amanda J. & Rickard, Claire M. (2019). Nurses' decision-making about intravenous administration set replacement: A qualitative study. Journal of Clinical Nursing, 28(21-22), 3786-3795.
Reiter, Keramet; Ventura, Joseph; Lovell, David; Augustine, Dallas; Barragan, Melissa; Blair, Thomas; Chesnut, Kelsie; Dashtgard, Pasha; Gonzalez, Gabriela; Pifer, Natalie & Strong, Justin (2020). Psychological distress in solitary confinement: Symptoms, severity, and prevalence in the United States, 2017-2018. American Journal of Public Health, 110(S1), S56-S62, https://doi.org/10.2105/ajph.2019.305375 [Accessed: October 1, 2022].
Roos, Anne Karine Østbye; Skaug, Eli Anne; Grøndahl, Vigdis Abrahamsen & Helgesen, Ann Karin (2020). Trading company for privacy: A study of patients' experiences. Nursing Ethics, 27(4), 1089-1102.
Roshanzadeh, Mostafa; Vanaki, Zohreh & Sadooghiasl, Afsaneh (2020). Sensitivity in ethical decision-making: The experiences of nurse managers. Nursing Ethics, 27(5), 1174-1186.
Roy, Monika; Bolton-Moore, Carolyn; Sikazwe, Izukanji; Mukumbwa-Mwenechanya, Mpande; Efronson, Emilie; Mwamba, Chanda; Somwe, Paul; Kalunkumya, Estella; Lumpa, Mwansa; Sharma, Anjali; Pry, Jake; Mutale, Wilbroad; Ehrenkranz, Peter; Glidden, David V.; Padian, Nancy; Topp, Stephanie; Geng, Elvin & Holmes, Charles B. (2020). Participation in adherence clubs and on-time drug pickup among HIV-infected adults in Zambia: A matched-pair cluster randomized trial. PLoS Medicine, 17(7), e1003116, https://doi.org/10.1371/journal.pmed.1003116 [Accessed: October 1, 2022].
Rubio-Navarro, Alfonso; García-Capilla, Diego José; Torralba-Madrid, Maria José & Rutty, Jane (2020). Decision-making in an emergency department: A nursing accountability model. Nursing Ethics, 27(2), 567-586.
Rushton, Kelly; Fraser, Claire; Gellatly, Judith; Brooks, Helen; Bower, Peter; Armitage, Christopher J.; Faija, Cintia; Welsh, Charlotte & Bee, Penny (2019). A case of misalignment: the perspectives of local and national decision-makers on the implementation of psychological treatment by telephone in the improving access to psychological therapies service. BMC Health Services Research, 19(1), 997, https://doi.org/10.1186/s12913-019-4824-4 https://doi.org/10.1371/journal.pmed.1003116 [Accessed: October 1, 2022].
Sabone, Motshedisi; Mazonde, Pelonomi; Cainelli, Francesca; Maitshoko, Maseba; Joseph, Renatha; Shayo, Judith; Morris, Baraka; Muecke, Marjorie; Mann Wall, Barbra; Hoke, Linda; Peng, Lilian; Mooney-Doyle, Kim & Ulrich, Connie M. (2020). Everyday ethical challenges of nurse-physician collaboration. Nursing Ethics, 27(1), 206-220.
Saei Ghare Naz, Marzieh; Ramezani Tehrani, Fahimeh; Ahmadi, Fazlollah; Alavi Majd, Hamid & Ozgoli, Giti (2019). Threats to feminine identity as the main concern of Iranian adolescents with polycystic ovary syndrome: A qualitative study. Journal of Pediatric Nursing, 49, e42-e47.
Salberg, Johanna; Bäckström, Josefin; Röing, Marta & Öster, Caisa (2019). Ways of understanding nursing in psychiatric inpatient care—A phenomenographic study. Journal of Nursing Management, 27(8), 1826-1834, https://doi.org/10.1111/jonm.12882 [Accessed: October 1, 2022].
Saleh, Mohammad Y.N.; Al-Amer, Rasmieh; Al Ashram, Safaa Radi; Dawani, Hania & Randall, Sue (2020). Exploring the lived experience of Jordanian male nurses: A phenomenological study. Nursing Outlook, 68(3), 313-323.
Salehi, Zahra; Najafi Ghezeljeh, Tahereh; Hajibabaee, Fatemeh & Joolaee, Soodabeh (2020). Factors behind ethical dilemmas regarding physical restraint for critical care nurses. Nursing Ethics, 27(2), 598-608.
Saranrittichai, Kesinee; Ussavapark, Wichai; Thamrongwarangkoon, Apisit; Haengsorn, Tiptiya; Daoruang, Sureerat & Teeranut, Ampornpan (2020). Community-based approaches to cancer prevention in rural Thailand based on experiences of accredited health professionals. Asian Pacific Journal of Cancer Prevention, 21(1), 7-12, https://doi.org/10.31557/apjcp.2020.21.1.7 [Accessed: October 1, 2022].
Sebayang, Susy K.; Dewi, Desak Made Sintha Kurnia; Lailiyah, Syifa’ul & Ahsan, Aabdillah (2019). Mixed-methods evaluation of a ban on tobacco advertising and promotion in Banyuwangi district, Indonesia. Tobacco Control, 28(6), 651-656.
Seidlein, Anna-Henrikje; Buchholz, Ines; Buchholz, Maresa & Salloch, Sabine (2020). Concepts of health in long-term home care: An empirical-ethical exploration. Nursing Ethics, 27(5), 1187-1200.
Seki, Masayasu; Fujinuma, Yasuki; Matsushima, Masato; Joki, Tatsuhiro; Okonogi, Hideo; Miura, Yasuhiko & Ohno, Iwao (2019). How a problem-based learning approach could help Japanese primary care physicians: a qualitative study. International Journal of Medical Education, 10, 232-240, https://doi.org/10.5116/ijme.5de7.99c7 [Accessed: October 1, 2022].
Semple, Cherith J.; Rutherford, Helen; Killough, Simon; Moore, Ciaran & McKenna, Gerry (2019). Long-term impact of living with an obturator following a maxillectomy: A qualitative study. Journal of Dentistry, 90, 103212.
Shahabuddin, A.S.M.; Sharkey, Alyssa B.; Jackson, Debra; Rutter, Paul; Hasman, Andreas & Sarker, Malabika (2020). Carrying out embedded implementation research in humanitarian settings: A qualitative study in Cox's Bazar, Bangladesh. PLoS Medicine, 17(7), e1003148, https://doi.org/10.1371/journal.pmed.1003148 [Accessed: October 1, 2022].
Sim, Ming Ann; Lee, Soo-Hoon; Phan, Phillip H. & Lateef, Aisha (2020). Quality improvement at an acute medical unit in an Asian academic center: A mixed methods study of nursing work dynamics. Nursing Outlook, 68(2), 169-183.
Skelton, Teresa; Irakoze, Alain; Bould, M. Dylan; Przybylak-Brouillard, Antoine; Twagirumugabe, Theogene & Livingston, Patricia (2020). Retention and migration of Rwandan anesthesiologists: A qualitative study. Anesthesia & Analgesia, 131(2), 605-612, https://doi.org/10.1213/ane.0000000000004794 [Accessed: October 1, 2022].
Srinivasan, Malathi; Asch, Steven; Vilendrer, Stacie; Thomas, Samuel Crandall; Bajra, Rika; Barman, Linda; Edwards, Lauren Michelle; Filipowicz, Heather; Giang, Lena; Jee, Olivia; Mahoney, Megan; Nelligan, Ian; Jayant Phadke, Anuradha; Torres, Elise & Artandi, Maja (2020). Qualitative assessment of rapid system transformation to primary care video visits at an academic medical center. Annals of Internal Medicine, 173(7), 527-535, https://doi.org/10.7326/m20-1814 [Accessed: October 1, 2022].
Strömbäck, Maria; Fjellman-Wiklund, Anncristine; Keisu, Sara; Sturesson, Marine & Eskilsson, Therese (2020). Restoring confidence in return to work: A qualitative study of the experiences of persons with exhaustion disorder after a dialogue-based workplace intervention. PLoS One, 15(7), e0234897, https://doi.org/10.1371/journal.pone.0234897 [Accessed: October 1, 2022].
Symanski, Elaine; An Han, Heyreoun; Hopkins, Loren; Smith, Mary Ann; McCurdy, Sheryl; Han, Inkyu; Jimenez, Maria; Markham, Christine; Richner, Donald; James, Daisy & Flores, Juan (2020). Metal air pollution partnership solutions: Building an academic-government-community-industry collaboration to improve air quality and health in environmental justice communities in Houston. Environmental Health, 19(1), 39, https://doi.org/10.1186/s12940-020-00590-1 [Accessed: October 1, 2022].
Timberlake, David S.; Laitinen, Ulla; Kinnunen, Jaana M.; & Rimpela, Arja H. (2020). Strategies and barriers to achieving the goal of Finland's tobacco endgame. Tobacco Control, 29(4), 398-404, https://doi.org/10.1136/tobaccocontrol-2018-054779 [Accessed: October 1, 2022].
Tompkins, Charlotte N.E.; Burnley, Annabel; McNeill, Ann & Hitchman, Sara C. (2020). Factors that influence smokers' and ex-smokers' use of IQOS: A qualitative study of IQOS users and ex-users in the UK. Tobacco Control, 30(1), 16-23, https://doi.org/10.1136/tobaccocontrol-2019-055306 [Accessed: October 1, 2022].
Urquhart, Robin; Kendell, Cynthia; Cornelissen, Evelyn; Madden, Laura L.; Powell, Byron J.; Kissmann, Glenn; Richmond, Sarah A.; Willis, Cameron & Bender, Jackie L. (2020). Defining sustainability in practice: Views from implementing real-world innovations in health care. BMC Health Services Research, 20(1), 87, https://doi.org/10.1186/s12913-020-4933-0 [Accessed: October 1, 2022].
Vanstone, Meredith; Neville, Thanh H.; Clarke, France J.; Swinton, Marilyn; Sadik, Marina; Takaoka, Alyson; Smith, Orla; Baker, Andrew J.; LeBlanc, Allana; Foster, Denise; Dhingra, Vinay; Phung, Peter; Xu, Xueqing (Sherry); Kao, Yuhan; Heels-Ansdell, Diane; Tam, Benjamin; Toledo, Feli; Boyle, Anne & Cook, Deborah J. (2020). Compassionate end-of-life care: Mixed-methods multisite evaluation of the 3 Wishes project. Annals of Internal Medicine, 172(1), 1-11.
Voogt, Judith J.; Kars, Marijke C.; van Rensen, Elizabeth L.J.; Schneider, Margriet M.E.; Noordegraaf, Mirko & van der Schaaf, Marieke F. (2020). Why medical residents do (and don't) speak up about organizational barriers and opportunities to improve the quality of care. Academic Medicine, 95(4), 574-581, https://doi.org/10.1097/acm.0000000000003014 [Accessed: October 1, 2022].
Vos, J., Franklin, B.D., Chumbley, G., Galal-Edeen, G.H., Furniss, D. & Blandford, A. (2020). Nurses as a source of system-level resilience: Secondary analysis of qualitative data from a study of intravenous infusion safety in English hospitals. International Journal of Nursing Studies, 102, 103468, https://doi.org/10.1016/j.ijnurstu.2019.103468 [Accessed: October 1, 2022].
Walburn, Jessica; Anderson, Rebecca & Morgan, Myfanwy (2020). Forms, interactions, and responses to social support: A qualitative study of support and adherence to photoprotection amongst patients with Xeroderma pigmentosum. British Journal of Health Psychology, 25(1), 89-106, https://doi.org/10.1111/bjhp.12396 [Accessed: October 1, 2022].
Warner, Nafisseh S.; Finnie, Dawn; Warner, David O.; Hooten, W. Michael; Mauck, Karen F.; Cunningham, Julie L.; Gazelka, Halena; Bydon, Mohamad; Huddleston, Paul M. & Habermann, Elizabeth B. (2020). The system is broken: A qualitative assessment of opioid prescribing practices after spine surgery. Mayo Clinic Proceedings, 95(9), 1906-1915.
Weller, C.D., Richards, C., Turnour, L., Patey, A.M., Russell, G. & Team, V. (2020). Barriers and enablers to the use of venous leg ulcer clinical practice guidelines in Australian primary care: A qualitative study using the theoretical domains framework. International Journal of Nursing Studies, 103, 103503.
Wheeler, Margaret; de Bourmont, Shalila; Paul-Emile, Kimani; Pfeffinger, Alana; McMullen, Ashley; Critchfield, Jeff M. & Fernandez, Alicia (2019). Physician and trainee experiences with patient bias. JAMA Internal Medicine, 179(12), 1678-1685.
Womack, Dana M.; Vuckovic, Nancy N.; Steege, Lindsey M.; Eldredge, Deborah H.; Hribar, Michelle & Gorman, Paul N. (2019). Subtle cues: Qualitative elicitation of signs of capacity strain in the hospital workplace. Applied Ergonomics, 81, 102893.
Zhao, Yali; Zhao, Xuexue; Liu, Yanli; Wei, Yun; Jin, Guanghui; Shao, Shuang & Lu, Xiaoqin (2019). Perceptions, behaviours, barriers and needs of evidence-based medicine in primary care in Beijing: A qualitative study. BMC Family Practice, 20(1), 171, https://doi.org/10.1186/s12875-019-1062-0 [Accessed: October 1, 2022].
1) The articles included in analysis are listed in the Appendix. Please contact James DuBOIS at duboisjm@wustl.edu to request the codebook and code application tables underlying this analysis. <back>
Alexander, Steven M.; Jones, Kristal; Bennett, Nathan J.; Budden, Amber; Cox, Michael; Crosas, Mercé; Game, Edward T.; Geary, Janis; Hardy, R. Dean; Johnson, Jay T.; Karcher, Sebastian; Motzer, Nicole; Pittman, Jeremy; Randell, Heather; Silva, Julie A.; da Silva, Patricia Pinto; Strasser, Carly; Strawhacker, Colleen; Stuhl, Andrew & Weber, Nic (2019). Qualitative data sharing and synthesis for sustainability science. Nature Sustainability, 3(2), 81-88.
Antes, Alison L.; Walsh, Heidi; Strait, Michelle; Hudson-Vitale, Cynthia R. & DuBois, James M. (2018). Examining data repository guidelines for qualitative data sharing. Journal of Empirical Research on Human Research Ethics, 13(1), 61-73, https://doi.org/10.1177/1556264617744121 [Accessed: October 1, 2022].
Ashley, Florence (2020). Accounting for research fatigue in research ethics. Bioethics, 35(3), 270-276.
Baker, John A.; Canvin, Krysia & Berzins, Kathryn (2019). The relationship between workforce characteristics and perception of quality of care in mental health: A qualitative study. International Journal of Nursing Studies, 100, 103412.
Barbour, Rosaline S. (2000). The role of qualitative research in broadening the "evidence base" for clinical practice. Journal of Evaluation in Clinical Practice, 6(2), 155-163.
Bishop, Libby (2006). A proposal for archiving context for secondary analysis. Methodological Innovation Online, 1(2), 10-20, https://doi.org/10.4256/mio.2006.0008 [Accessed: October 1, 2022].
Bishop, Libby (2009). Ethical sharing and reuse of qualitative data. Australian Journal of Social Issues, 44(3), 255-272.
Bishop, Libby (2014). Re-using qualitative data: A little evidence, on-going issues and modest reflections. Studia Socjologiczne, 3, 167-176.
Bishop, Libby & Kuula-Luumi, Arja (2017). Revisiting qualitative data reuse. SAGE Open, 7(1), https://doi.org/10.1177/2158244016685136 [Accessed: October 1, 2022].
Broom, Alex; Cheshire, Lynda & Emmison, Michael (2009). Qualitative researchers' understandings of their practice and the implications for data archiving and sharing. Sociology, 43(6), 1163-1180.
Carusi, Annamaria & Jirotka, Marina (2009). From data archive to ethical labyrinth. Qualitative Research, 9(3), 285-298.
Chatfield, Sheryl L. (2020). Recommendations for secondary analysis of qualitative data. The Qualitative Report, 25(3), 833-842, https://doi.org/10.46743/2160-3715/2020.4092 [Accessed: October 1, 2022].
Chukwuma, Adanna; Gong, Estelle; Latypova, Mutriba & Fraser-Hurt, Nicole (2019). Challenges and opportunities in the continuity of care for hypertension: A mixed-methods study embedded in primary health care intervention in Tajikistan. BMC Health Services Research, 19, 925, https://doi.org/10.1186/s12913-019-4779-5 [Accessed: October 1, 2022].
Corti, Louise (2000). Progress and problems of preserving and providing access to qualitative data for social research —The international picture of an emerging culture. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 1(3), Art. 2, https://doi.org/10.17169/fqs-1.3.1019 [Accessed: October 1, 2022].
Corti, Louise (2007). Re-using archived qualitative data—where, how, why?. Archival Science, 7(1), 37-54, https://doi.org/10.1007/s10502-006-9038-y [Accessed: October 1, 2022].
Davies, A.R.; Homolova, L.; Grey, C.N.B. & Bellis, M.A. (2019). Health and mass unemployment events-developing a framework for preparedness and response. Journal of Public Health (Oxf), 41(4), 665-673, https://doi.org/10.1093/pubmed/fdy174 [Accessed: October 1, 2022].
Dickson-Swift, Virginia; James, Erica L.; Kippen, Sandra & Liamputtong, Pranee (2006). Blurring boundaries in qualitative health research on sensitive topics. Qualitative Health Research, 16(6), 853-871.
DuBois, James M.; Strait, Michelle & Walsh, Heid (2018). Is It time to share qualitative research data?. Qualitative Psychology, 5(3), 380-393, https://doi.org/10.1037/qup0000076 [Accessed: October 1, 2022].
Elman, Colin; Kapiszewski, Diana & Kirilova, Dessislava (2014). Learning through research: Using data to train undergraduates in qualitative methods. PS: Political Science & Politics, 48(01), 39-43.
Feldman, Shelley & Shaw, Linda (2019). The epistemological and ethical challenges of archiving and sharing qualitative data. American Behavioral Scientist, 63(6), 699-721.
Guillemin, Marilys & Heggen, Kristin (2009). Rapport and respect: Negotiating ethical relations between researcher and participant. Medicine, Health Care and Philosophy, 12(3), 291-299, https://doi.org/10.1007/s11019-008-9165-8 [Accessed: October 1, 2022].
Gupta, Aditi; Lai, Albert; Mozersky, Jessica; Ma, Xiaoteng; Walsh, Heidi & DuBois, James M. (2021). Enabling qualitative data sharing using a natural language processing pipeline for de-identification: Moving beyond HIPAA safe harbor identifiers. JAMIA Open, 4(3), 1-10, https://doi.org/10.1093/jamiaopen/ooab069 [Accessed: October 1, 2022].
Hammersley, Martyn (2010). Can we re-use qualitative data via secondary analysis? Notes on some terminological and substantive issues. Sociological Research Online, 15(1), 47-53.
Kapiszewski, Diana & Kirilova, Dessislava (2014). Transparency in qualitative security studies research: Standards, benefits, and challenges. Security Studies, 23, 699-707.
Karcher, Sebastian; Kirilova, Dessislava; Pagé, Christiane & Weber, Nic (2021). How data curation enables epistemically responsible reuse of qualitative data. The Qualitative Report, 26(6), 1996-2010, https://doi.org/10.46743/2160-3715/2021.5012 [Accessed: October 1, 2022].
Kirilova, Dessislava & Karcher, Sebastian (2017). Rethinking data sharing and human participant protection in social science research: Applications from the qualitative realm. Data Science Journal, 16, 43, https://doi.org/10.5334/dsj-2017-043 [Accessed: October 1, 2022].
Kuula, Arja (2011). Methodological and ethical dilemmas of archiving qualitative data. IASSIST Quarterly, 34(3-4), 12-17, https://doi.org/10.29173/iq455 [Accessed: October 1, 2022].
Levenstein, Margaret C. & Lyle, Jared A. (2018). Data: Sharing is caring. Advances in Methods and Practices in Psychological Science, 1(1), 95-103, https://doi.org/10.1177/2515245918758319 [Accessed: October 1, 2022].
Li, Huanhuan; Sun, Dan; Wan, Zhenzhen; Chen, Jialu & Sun, J. (2020). The perceptions of older nurses regarding continuing to work in a nursing career after retirement: A qualitative study in two Chinese hospitals of different levels. International Journal of Nursing Studies, 105, 103554.
Lupia, Arthur & Elman, Colin (2013). Openness in political science: Data access and research transparency. PS: Political Science & Politics, 47(01), 19-42.
Mannheimer, Sara; Pienta, Amy; Kirilova, Dessislava; Elman, Colin & Wutich, Amber (2019). Qualitative data sharing: Data repositories and academic libraries as key partners in addressing challenges. American Behavioral Scientist, 63(5), 643-664, https://doi.org/10.1177/0002764218784991 [Accessed: October 1, 2022].
McLellan, Eleanor; MacQueen, Kathleen M. & Neidig, Judith L. (2016). Beyond the qualitative interview: Data preparation and transcription. Field Methods, 15(1), 63-84.
Moore, Niamh (2006). The contexts of context: Broadening perspectives in the (re)use of qualitative data. Methodological Innovation Online, 1(2), 21-32, https://doi.org/10.4256/mio.2006.0009 [Accessed: October 1, 2022].
Mozersky, Jessica; Friedrich, Annie B. & DuBois, James M. (2022). A content analysis of 100 qualitative health research articles to examine researcher-participant relationships and implications for data sharing. International Journal of Qualitative Methods, 21, https://doi.org/10.1177/16094069221105074 [Accessed: October 1, 2022].
Mozersky, Jessica; McIntosh, Tristan; Walsh, Heidi; Parsons, Meredith V.; Goodman, Melody & DuBois, James M. (2021). Barriers and facilitators to qualitative data sharing in the United States: A survey of qualitative researchers. PLOS One, 16(12), e0261719, https://doi.org/10.1371/journal.pone.0261719 [Accessed: October 1, 2022].
Mozersky, Jessica; Parsons, Meredith; Walsh, Heidi; Baldwin, Kari; McIntosh, Tristan & DuBois, James M. (2020). Research participant views regarding qualitative data sharing. Ethics & Human Research, 42(2), 13-27, https://doi.org/10.1002/eahr.500044 [Accessed: October 1, 2022].
Mozersky, Jessica; Walsh, Heidi; Parsons, Meredith; McIntosh, Tristan; Baldwin, Kari & DuBois, James M. (2020). Are we ready to share qualitative research data? Knowledge and preparedness among qualitative researchers, IRB members, and data repository curators. IASSIST Quarterly, 43(4), 1-23, https://doi.org/10.29173/iq952 [Accessed: October 1, 2022].
National Institutes of Health (2020). NIH data sharing policy and implementation guidance. U.S. Department of Health and Human Services, https://grants.nih.gov/grants/policy/data_sharing/data_sharing_guidance.htm [Accessed: October 1, 2022].
Nosek, B.A.; Alter, G.; Banks, G.C.; Borsboom, D.; Bowman, S.D.; Breckler, S.J.; Buck, S.; Chambers, C.D.; Chin, G.; Christensen, G.; Contestabile, M.; Dafoe, A.; Eich, E.; Freese, J.; Glennerster, R.; Goroff, D.; Green, D.P.; Hesse, B.; Humphreys, M.; Ishiyama, J.; Karlan, D.; Kraut, A.; Lupia, A.; Mabry, P.; Madon, T.; Malhotra, N.; Mayo-Wilson, E.; McNutt, M.; Miguel, E.; Levy Paluck, E.; Simonsohn, U.; Soderberg, C.; Spellman, B.A.; Turitto, J.; VandenBos, G.; Vazire, S.; Wagenmakers, E.J.; Wilson, R. & Yarkoni, T. (2015). Promoting an open research culture. Science, 348(6242), 1422-1425.
Ohayon, Jennifer Liss; Nost, Eric; Silk, Kami; Rakoff, Michele & Brody, Julia Green (2020). Barriers and opportunities for breast cancer organizations to focus on environmental health and disease prevention: A mixed-methods approach using website analyses, interviews, and focus groups. Environmental Health, 19(1), 15, https://doi.org/10.1186/s12940-020-0570-7 [Accessed: October 1, 2022].
Reiter, Keramet; Ventura, Joseph; Lovell, David; Augustine, Dallas; Barragan, Melissa; Blair, Thomas; Chesnut, Kelsie; Dashtgard, Pasha; Gonzalez, Gabriela; Pifer, Natalie & Strong, Justin (2020). Psychological distress in solitary confinement: Symptoms, severity, and prevalence in the United States, 2017-2018. American Journal of Public Health, 110(S1), S56-S62, https://doi.org/10.2105/ajph.2019.305375 [Accessed: October 1, 2022].
Taichman, Darren B.; Backus, Joyce; Baethge, Christopher; Bauchner, Howard; de Leeuw, Peter W.; Drazen, Jeffrey M.; Fletcher, John; Frizelle, Frank A.; Groves, Trish; Haileamlak, Abraham; James, Astrid; Laine, Christine; Peiperl, Larry; Pinborg, Anja; Sahni, Peush & Wu, Sinan (2016). Sharing clinical trial data: A proposal from the international committee of medical journal editors. Annals of Internal Medicine, 164, 505-506, https://doi.org/10.7326/m15-2928 [Accessed: October 1, 2022].
Tolich, Martin (2004). Internal confidentiality: When confidentiality assurances fail relational informants. Qualitative Sociology, 27(1), 101-106, https://doi.org/10.1023/B:QUAS.0000015546.20441.4a [Accessed: October 1, 2022].
Tsai, Alexander C.; Kohrt, Brandon A.; Matthews, Lynn T.; Betancourt, Theresa S.; Lee, Jooyoung K.; Papachristos, Andrew V.; Weiser, Sheri D. & Dworkin, Shari L. (2016). Promises and pitfalls of data sharing in qualitative research. Social Science & Medicine, 169, 191-198.
UK Data Service (2023). Anonymising qualitative data, https://ukdataservice.ac.uk/learning-hub/research-data-management/anonymisation/anonymising-qualitative-data/ [Accessed: October 1, 2022].
VandeVusse, Alicia; Mueller, Jennifer & Karcher, Sebastian (2022). Qualitative data sharing: Participant understanding, motivation, and consent. Qualitative Health Research, 32(1), 182-191, https://doi.org/10.1177/10497323211054058 [Accessed: October 1, 2022].
Vanstone, Meredith; Neville, Thanh H.; Clarke, France J.; Swinton, Marilyn; Sadik, Marina; Takaoka, Alyson; Smith, Orla; Baker, Andrew J.; LeBlanc, Allana; Foster, Denise; Dhingra, Vinay; Phung, Peter; Xu, Xueqing (Sherry); Kao, Yuhan; Heels-Ansdell, Diane; Tam, Benjamin; Toledo, Feli; Boyle, Anne & Cook, Deborah J. (2020). Compassionate end-of-life care: Mixed-methods multisite evaluation of the 3 Wishes project. Annals of Internal Medicine, 172(1), 1-11.
Warner, Nafisseh S.; Finnie, Dawn; Warner, David O.; Hooten, W. Michael; Mauck, Karen F.; Cunningham, Julie L.; Gazelka, Halena; Bydon, Mohamad; Huddleston, Paul M. & Habermann, Elizabeth B. (2020). The system is broken: A qualitative assessment of opioid prescribing practices after spine surgery. Mayo Clinic Proceedings, 95(9), 1906-1915.
Wheeler, Margaret; de Bourmont, Shalila; Paul-Emile, Kimani; Pfeffinger, Alana; McMullen, Ashley; Critchfield, Jeff M. & Fernandez, Alicia (2019). Physician and trainee experiences with patient bias. JAMA Internal Medicine, 179(12), 1678-1685.
Yardley, Sarah J.; Watts, Kate M.; Pearson, Jennifer & Richardson, Jane C. (2014). Ethical issues in the reuse of qualitative data: Perspectives from literature, practice, and participants. Qualitative Health Research, 24(1), 102-113.
Yoon, Ayoung (2014). "Making a square fit into a circle": Researchers' experiences reusing qualitative data. Proceedings of the American Society for Information Science and Technology, 51(1), 1-4, https://doi.org/10.1002/meet.2014.14505101140 [Accessed: October 1, 2022].
|
Annie FRIEDRICH is an assistant professor of bioethics and medical humanities in the Institute for Health & Equity at the Medical College of Wisconsin. In her research, she combines theoretical and empirical analyses to explore the ethical dimensions of clinical care, family-provider communication, and decision making in pediatric settings. She is also an ethics educator and teaches bioethics to medical students, graduate students, and other health professionals. |
Contact: Dr. Annie Friedrich Medical College of Wisconsin E-mail: afriedrich@mcw.edu |
|
Jessica MOZERSKY is an assistant professor of medicine in the Bioethics Research Center at Washington University School of Medicine in St. Louis, Missouri. She is a qualitative researcher who conducts empirical research on the ethical and social implications of returning genetic and imaging results to research participants, informed consent, and data sharing. |
Contact: Dr. Jessica Mozersky Bioethics Research Center E-mail: jmozersky@wustl.edu |
|
James DuBOIS is the Bander professor of medical ethics and director of the Bioethics Research Center at Washington University School of Medicine in St. Louis, Missouri. He is an editor-in-chief of Narrative Inquiry in Bioethics: A Journal of Qualitative Research. In his research, he uses social science methods to examine ethical and social issues surrounding the use of new technologies, informed consent to clinical trials, data sharing, and organ transplantation. |
Contact: Dr. James M. DuBois Bioethics Research Center E-mail: duboisjm@wustl.edu |
Friedrich, Annie B.; Mozersky, Jessica & DuBois, James M. (2023). Potentially identifying variables reported in 100 qualitative health research articles: Implications for data sharing and secondary analysis [33 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 24(2), Art. 18, https://dx.doi.org/10.17169/fqs-24.2.3965.