

Volume 5, No. 1, Art. 17 – January 2004
Making Decisions About Taking Medicines: A Social Coordination Process
Amrei C. Joerchel & Jaan Valsiner
Abstract: How do people decide to take medication? When is it necessary to do something about the condition one is in when falling ill? These questions require answers at two levels—first at the general decision structure of what features of thinking processes are coordinated to make the decision (the macrogenetic model), and how the actual decision process works individually (the microgenetic model). Both models are described, and selected case analyses from an interview study of 25 young adults are presented. Based on the evidence we show that each and every subject makes use of the same macrogenetic and microgenetic models. Our evidence also shows that the folk model—"the body as a machine"—is present in every interview. Such general folk models frame the intricate decision making process between the microgenetic and macrogenetic levels. The act of taking medicine while facing a minor impending illness is a complex psychological process described and discussed in this paper.
Key words: medication, illnesses, decision making, cognitive heuristics, macrogenetic and microgenetic processes
Table of Contents
1. Introduction
2. Meanings of Medicines, Cognitive Heuristics and Affective Decision Making
2.1 The macrogenetic and microgenetic models
2.2 Two levels of analysis
2.3 Elaboration of the model for the microgenetic process
2.4 Elaboration of the macrogenetic process
2.5 The arena of parole-langue relation as the locus of inter-levels dialogue
3. Method
3.1 Materials
3.2 Subjects
3.3 Procedure
3.4 Analyzing the interviews
4. Results
4.1 Data summary
4.2 Reasons for taking medicines
4.3 Data analysis subject 23: Myths and memories that guide decision making
4.4 Data analysis subject 2: Ambivalence about taking medication
5. Discussion
Falling ill and getting better belongs to human life as much as sleeping, eating and making friends. The process of falling ill and getting better is as old as mankind itself—without overcoming illnesses our species would not have survived. Only recently have persons discovered and taken advantage of the use of certain medications that, while being effective, create biological dangers for the body. Today, taking one or another kind of medicine is a common phenomenon in any human society. The phrase "Why don't you take some Tylenol1)" is only too familiar. [1]
And yet, how does a person actually decide to take medicine? This simple question leads to the question—unsolved by basic cognitive science—of how the process of decision making is organized within irreversible time. It is a process filled with ambiguity (see ABBEY & VALSINER, 2003). The person is constantly in a two-way relation with the immediate environment. In the case of the issue at stake here—taking medicine—that environment is the person's own body—the Subject (agentive Person) reflects upon the Object (the Person's own Body). This intra-personal process is inherently ambiguous: the Person feels that something is "not quite right" with the Body, but cannot precisely say what it is ("I seem to be falling ill"). Furthermore, this present ambiguous relationship relates to the expectation for the immediate future relation of the Person with Body ("Maybe tomorrow I am completely ill" ... but "maybe not"). Thus, any decision about taking medicine at any here-and-now setting needs to coordinate two ambiguities. In order to do that, the Person imports into the situation pre-existing knowledge (about illnesses, medicines, their effects and side effects, advices by specialists and close persons, etc). The Person creates hierarchical structures of semiotic mediating devices for the handling of the current problem situation (VALSINER, 2001). Once such hierarchy does its job it may be demolished as the person continues one's everyday activities. Yet some personal-cultural memory trace is preserved—to be retrieved later in similar situations when the reduction of uncertainty is needed. [2]
How is it that people decide to take an active step towards either preventing or curing an illness or simply treating bodily discomfort? In the previous study (JOERCHEL, 2002) it was concluded that the precise moment in which people decide to take any sort of medication varies from individual to individual according to their personal meaning system. Yet the major issue remains—what does it mean to take medicine? A person may think: "How will it affect my body, my psyche and or in general, how will it affect me?" [3]
2. Meanings of Medicines, Cognitive Heuristics and Affective Decision Making
What is medication—all the pills, lotions, powders that some social role carrier—the medical expert, shaman, or pharmacist—make available to us. Medicines are a category of substances that is located in some relation to the category of foods on the one end, and poisons on the other. It is a fluid category—a field of substances that under some circumstances becomes united with that of poisons, at others—with that of foods. Thus, we can observe a dynamic picture of meaning-making:
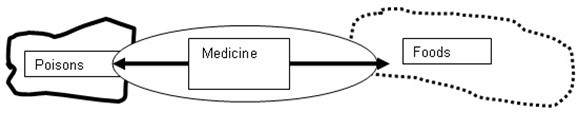
Any substance that our bodies can take in can be located at the intersection where the fluid category of medicines is—and
the tension between the two poles leads the dynamic re-definition of different foods into medicine (e.g., as in efforts to cure or prevent diseases by diets, special foods, etc), or medicines into poisons (as a result of increasing side-effects of a medicine, the body perceives it as a poison)—and withdrawn from the market (e.g., the Thalidomide or Baycol cases). The given substance can move over its history of
uses widely between the three states: consider the use of tobacco as food, as medicine—and as poison (in our contemporary
world where the "war on smoking" is having its increasing crowds of naive followers). From a biological standpoint it is some
chemical substance that is taken into the body in parallel with other substances—such as foods (and food additives) or drinks.
The meaning of medicines is different from regularly taken chemicals. [4]
The picture painted above is admittedly that of cultural history— the collective-cultural tension about the meaning of medicines. However, the focus in this paper is that of personal-cultural kind. Any chemical we take in at any time can in principle be poisonous (e.g. overdose of sleeping pills) or non-poisonous and functional (e.g. a normal dose of the same pills). A new medicine the doctor recommends to me given my current health problem may cure it—or kill me (due to the unpredictable "interaction effects" that particular substance has with previously used medicines that still are deposited in the body. Equally possibly the substance creates a psychological illusion that may work for me in some unspecified way ("placebo effect"), together with the organismic power of my body to heal itself. However, at the moment of the decision to take the particular medicine the actual outcome of using that medicine is not known to anybody. Its effects can be predicted as to their general direction, but not in their specifics. There is always uncertainty as to the what place the given substance occupies—already at the biochemical level—on the food-medicine-poison system for my body at the given time. [5]
The computational capacities of the human mind are constrained when making decisions under the pressures of acting within the irreversible time. Furthermore, in the face of most everyday life problems being those of ill-defined kind (SIMON & NEWELL, 1982 p.384). The goals of the person who is in the process of falling ill (or thinks so) are not well set, not unitary. The illness is impending—but it might also pass without intervention. The illness may look uncomfortable—but bearable—especially if the person is used to avoiding taking medicine. Or the illness may be so threatening that the person has been taking medicine regularly to prevent it (e.g., the popular lore that taking an aspirin a day keeps an infarction away). Different persons set up their orientation in the middle of such ill-defined problem situations. [6]
Furthermore, any person's perception, attention, memories and information-processing capabilities are limited when operating under time constraints. In the evolutionary past it has been highly beneficial for humans to resort to simplifying rules and heuristics, rather than trying to expand these limitations. It has been argued that fast and frugal heuristics are tools that work remarkably well because they exploit structural regularities in the environment (GIGERENZER et al., 1999). The resulting—crude but sufficient mental tools—Fast and Frugal Heuristics (FFH)—rely on three simple building blocks—means for guiding search, means for stopping search, and means for decision making—thus, the mental tools do not use full computing algorithms, rather, they only search for the particular information needed (GINZBERG & KURZENHAUSER, 2004). Since the capacities of the human mind are limited in many ways, the usage of such fast tools is highly beneficial and therefore of adaptive quality in human evolution. Searching for key elements instead of for knowledge about a specific instance as a whole speeds up the process remarkably and thereby enables the individual to come to a set decision much faster. [7]
However, our decision making is not primarily rational but affective. While GIGERENZER et al. (1999) have developed a sophisticated notion of heuristics based on speedy mental processes, MELLERS et al. (2001) have addressed the importance of the social and emotional world as well. According to MELLERS et al., both of these aspects (the social as well as the emotional) influence the heuristics that persons will use in their decision making. Falling ill is not an affect-neutral event—it is usually a distracter for one's life-space events. The ambiguities triggered there are affect-laden. Persons contemplate what will happen when they do take some medicine—as well as what will happen if they do not. They ask how they feel at the moment, how they have felt in the past and how they will feel in the future. They may feel bad for themselves, or worry about what their loved ones feel if they tell them about the impending illness—especially a seriously life-threatening one. While emotions are essential in decision-making, social processes are equally important. [8]
Individual decision processes of medication are guided by collective-cultural myth stories about health issues that circulate in the given society. The reoccurrence of the usage of myths when persons decide to take medication further supports MELLERS et al. emphasis of the social influence on individuals. Myths, as stories about unverifiable historical events, function as mediating devices within which personal cultures are directed in one way or another (GUPTA & VALSINER, 1996). The main context of a story is worked through and processed by the listener as well as by the teller. If a person hears a myth about for example antibiotics not helping the body get well, but rather the body simply creating a higher immunity to it, the individual will work through the relationship of antibiotics and the body and will then, according to whether the listener actually believes the story or not, form an opinion about antibiotics. If he believes the story he will have a negative impression of antibiotics, whereas he will be more in favor for them if he does not believe the myth. Whether he believes the story or not, the listener will have been confronted with the issue and will have formed an opinion accordingly. Myths and stories greatly influence the person from a social aspect while he or she creates a personal meaning system. [9]
2.1 The macrogenetic and microgenetic models
Heuristics—problem-solving mechanisms of either computational or fast and frugal nature—do not exclude emotional, cultural or social aspects (MELLERS et al., 1999), which influence an individual when he or she is making a decision about whether (and when) to take a medicine. However, science cannot solve the problem of how decisions about medication are made by simply attributing causality for those to one or another kind of heuristic (e.g., "John takes aspirin as he fuses a FFH" or "... as he uses the availability heuristic"), The decision process for taking medication needs an analysis of the actual processes of feeling and thinking as those occur in the person's subjective world. [10]
We posit a two level organization of that process. At a general level, cultural beliefs, personal beliefs, past experiences, memories and future anticipations are considered. The model describing these beliefs and emotions we call the macrogenetic model. At the immediate decision level, assessments about the bodily discomfort are important. In my conceptualization we have created a systemic picture that we call the microgenetic model. When an individual experiences a bodily discomfort, he will reflect on how he is feeling emotionally, assess what this discomfort might mean from a cultural perspective and compare and contrast it to social aspects. What does it mean to feel ill? In what way does it affect the emotional stability of a person? How has this emotional instability been treated in the culture? How do other persons in the culture view an ill person? What does it mean socially to be in discomfort? [11]
MELLERS et al. (1999) argue that these questions play as much of an important role in the heuristics of a person as do the cognitive aspect. A person does not simply reflect on past experiences and memories, humans are highly social persons and will be influenced by more aspects than simple cognitive tools. While heuristics are fast and frugal shortcuts for the human mind when making decisions, they never the less are highly complicated and need further analysis. The macrogenetic and microgenetic models described in this paper is a way to clearly bring out the problem-solving mechanisms persons use when facing the problem of whether to take medication or not. [12]
While some have no problem with taking in a substance for any bodily discomfort, others do not even contemplate such an idea. Even though the previous study (JOERCHEL, 2002) highlighted how different persons feel about taking medication, it has further led us to recognize that they must all go through the same macrogenetic as well as microgenetic process of internalizing some sort of idea of what medicine will do for a person when she or he is in a situation of bodily discomfort. [13]
Each individual goes through an internalizing/externalizing process while making sense of any new feature of one's relations with the environment (VALSINER, 1997, Chapter 8). Such process is notable when the taking of medication becomes an issue. A person does this simultaneously at two levels. The macrogenetic process involves relating with beliefs and meanings (of the illness, of the medicines) that are already present in a society. These notions are integrated into the personal culture and stressed through the internalization/externalization process. This constitutes the basis for background for the microgenetic process. [14]
The microgenetic process depends on the individual's personal culture as it unfolds in a here-and-now setting. This process is based on a belief that has been created by the individual through past experiences, present needs, and future goals. For example, a person has established a general belief: "Prozac helps people overcome depression". When entering a depression, she or he may demand Prozac from the doctor—who may be reluctant to prescribe it. While personal cultures are influenced by external conditions—what a doctor might recommend, or not; what they hear from others—they are not part of a belief held in the society. The actual decision process of taking (or not taking) medicine only unfolds within the particular individual on the basis of various beliefs internalized by that person. [15]
An individual coordinates the macrogenetic and microgenetic processes in order to come to a clear-cut decision of whether to take medication or not. It is easy to imagine a person who has suffered bronchitis many times and believes that the only way to overcome this illness is by taking antibiotics. The same individual might very well be aware of the widely held notion that antibiotics are overridden and that your body will eventually become immune to the substance if taken too often. The person will try to justify his actions of taking them by using the internalized meaning system of the personal culture that has been established through previous lived-through experiences and believing that they are the only way of curing bronchitis. [16]
In contrast, consider a person with no substantial illness experience. A person who has never had bronchitis and who has not experienced the consequences of not taking antibiotics, yet who is very much aware of doctors being quick to prescribe antibiotics for almost everything, might go against the doctors recommendation and seek alternative options. Such person might explore several options and only after finding that none have cured the illness, try antibiotics. In this case the action will be justified by the person internally by reasoning that the individual has tried alternatives and even though the main cultural belief is that a body will form immunity towards such medication, the benefits are greater than the losses and as long as antibiotics are taken with caution it will by ok. Thus, both examples will use internalized meaning systems to justify their actions which go against the greater cultural belief of antibiotics being bad. [17]
2.3 Elaboration of the model for the microgenetic process
The microgenetic model depicts various ways of thinking that people use when feeling the need to either cure a bodily discomfort or prevent an illness (see Figure 1).
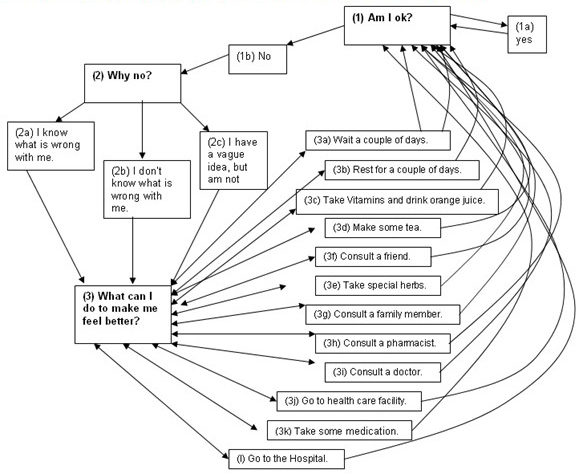
Figure 1: The microgenetic model [18]
The model uses various steps a person takes to ultimately always arrive at the same outcome—which is also the starting point for new decisions "Am I feeling fine?" [19]
Thus the first step (1) in this process is asking the question: "Am I ok?" If this question is answered with a "yes" (1a), then the person immediately returns to the starting questions and will be inclined to ask it again. In other words, choosing yes as an answer would close the circle of the microgenetic process right away. Is the question answered with a "no" (1b), further analysis is needed, which leads to the next step (2): "Why am I not ok? What is wrong with me?" Here the person will either take on the belief that he knows why he is feeling ill (2a), or he will not know (2c), or, a third option will be that he has a vague idea but is not sure about it (2c). This leaves the individual with three options, from which each of them will lead to a further step in his heuristics. Whether the person knows what is wrong or not, the next question will be what to do about the discomfort (3). The answer of this question depends largely on the previous answer of whether the person knows what is wrong or not, but also on the person's past experiences, on ones personal culture as well as on the macrogenetic model. [20]
Thus, while all persons go through the same heuristics in steps one and two, solving the third step will highly vary from individual to individual. The third stage of the microgenetic model consists of multiple options that are categorized from (a) to (k). A person might decide to wait a couple of days (3a) before doing anything else to see whether the illness will persist or get better. The second option is to actively take a couple of days rest (3b). The third category entails taking vitamins and drinking lots of orange juice (3c), and the fourth one is making some tea (3d), or ingesting any kind of special herb (3e), that would in some way sooth the discomforted body. One might also decide to consult a friend (3f), a family member (3g), or some authoritative figure such as a pharmacist (3h) or a doctor (3i). Or a person could decide to go to a health care facility (3j) to be checked out by either a nurse or a doctor. If the person believes to know what causes the discomfort, taking some medication (3k) is a plausible choice. Going to a hospital (3l) right away becomes an option when the person either does not know what is wrong and panics, or when a person does know what is wrong and also knows that such an illness or bodily discomfort is treated best in such a facility. [21]
One must not necessarily choose only one of the above options in stage three; it is probable that a combination of two or more is chosen. In other words, a person might decide to rest for a couple of days (3b), take some vitamins (3c), and consult a friend (3f). Or he might choose to only consult a doctor (3i). [22]
The third question poses a variety of options that can be chosen and if the choice results in a positive manner (no bodily discomfort is felt) the model will be closed by returning to step (1). If the person feels worse after completing the third step in his heuristic he will go back to the third question and try to answer it in a more sufficient way. So if a person has decided to wait a couple of days and realizes that his discomfort is either getting worse or simply persisting, he or she will ask again what he can do to make himself feel better. Individuals will go back and forth between this question and the various choices in the third stage of this model until he or she feels better and returns to the first question. How long this process takes place depends mostly on how severe the illness is, but also on the individual's personal meaning system, how it is made up, and in which ways the macrogenetic model sets the stage for concrete decisions by that individual. [23]
2.4 Elaboration of the macrogenetic process
A macrogenetic depicts general beliefs that are present in the whole society, past experiences of the individual and present assessments about necessary actions to be taken, what other individuals in the persons social group think, and future anticipations (see Figure 2).
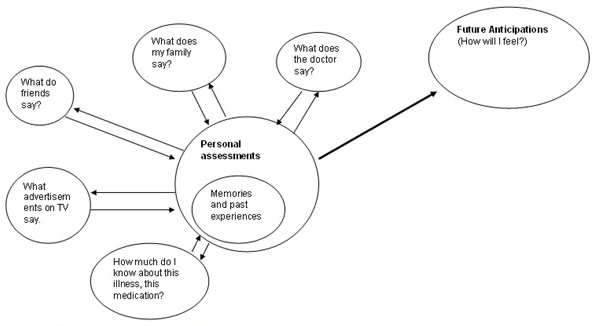
Figure 2: The macrogenetic model [24]
Collective-cultural beliefs are notions that are widely held by individuals of a particular society. The belief that medication will alter the state of one's present bodily condition is an example for how persons in Western culture perceive medicines. While individuals will differ in the degree to how much medicine will positively, or at the other end of the spectrum negatively, affect one's body, the notion that medication will in one way or another affect one's health influences the individual's personal cultural belief. The media is a powerful regulator for such beliefs. Commercials on TV and advertisements in magazines and newspapers are present in Western society in everyone's daily life and have an enormous affect on the individual and how he or she will decide to take or not to take medication. [25]
Since people of a particular society are subjected to the same media, they are influenced by the same ideas. Even though each individual will interpret these notions in terms of their existing knowledge of a product, past experiences and personal cultures, the notion is present throughout the whole society. Thus, a doctor, who is better informed about, for example, how antihistamines affect the body, will interpret a commercial for allergy medication in a very different manner than someone who has no medical background and has never dealt with allergies before. Yet, simply by being subjected to the same commercial, both will form some sort of belief about allergy medication. In some sense commercials and advertisements in a given society function in the same way as myths and folk stories do. They tell a certain story and individuals from the whole society work through the story that is told by listening to the commercials or reading the advertisements. [26]
Besides being affected by cultural beliefs that are omnipresent in a person's life, the individual will reflect on his or her experiences. So where a doctor might have professional knowledge about antihistamines and various allergy medications, an individual might have had severe problems with allergies in the past and will use these experiences when interpreting the cultural notion of allergy medication. The individuals will view the same commercial and remember what the medication did for him and then use past experiences to create his personal belief about the product. [27]
Another factor influencing the personal culture is how the individual assesses the present situation. In other words, what is going on in a person's life? Besides the starting question of how one feels, what one needs to do goes hand in hand with the previous one. Once the person experiences bodily discomfort, the question frequently turns into whether the daily activity of that person becomes impaired by that discomfort. What a person needs to do at the time he or she feels ill will greatly influence the decision of whether to take medication or not. [28]
Future anticipations play an equally important role in how an individual will decide what to do about the felt distress. If a person believes that taking antihistamines will eliminate hay-fever and other allergic reactions, he or she is inclined to take allergy medication, whereas persons who do not think that the medication will relieve the discomfort will be less likely to do so. Thus, how the person perceives future outcomes of either taking medication or not, influences the decision of what to do about such distress. [29]
Besides the collective-cultural and personal beliefs, what other persons in an individual's social life think influence that individual as well. These people can be family members, friends, or also authoritative figures such as doctors and nurses. Who influences the individual will vary from person to person. Yet, since humans are very sociable, other members of a social group play an important role in everyone's life and will influence the individual while making decisions. [30]
2.5 The arena of parole-langue relation as the locus of inter-levels dialogue
The threefold analytic scheme of langage, langue, and parole introduced by Ferdinand de SAUSSURE helps in the understanding of the interaction of the macrogenetic and the microgenetic model (VALSINER, 1998, pp.234-282):
Langage is simultaneously a social institution (e.g., such as French language) and human possibility (e.g., a capability of a person to utilize the language). In this respect, langage constitutes a duality between social and linguistic structures;
Langue refers to the domain of signs as those serve as linkages between thought and speaking activity; those signs are collective models taken over from langage by persons and stored in memory, and which become the basis for construction of thought through verbal means. Langue operates as a system of constraints (in the restrictive sense) upon the speaking activity.
Parole is the constructive activity of speaking and thinking, constrained by the person's langue-limits but expressing novel sentiments at each moment. It is a personal, incidental speaking act that reflects the acts of willing and intelligence, and leads to re-construction of langue (VALSINER, 1998, pp.255-256). [31]
In this scheme sign-regulated activities are mapped out in the following way. While langage sets the societal stage for the unity of langue and parole within a person, the passive, resultant collectivity of langue within a person is oppositionally and inseparably linked with the active process of parole. While VALSINER (1998, p.257) points out that the relation between langue and parole can be viewed as a dialogical process that exists due to the unavoidable uncertainty that exists in any speaking context, the helpfulness of this scheme for understanding the interaction between the macrogenetic and the microgenetic model used for decision making about taking medication lies in the relationship between langage (macrogenetic level) and the unity of langue and parole (microgenetic level). [32]
When talking about a person operating at the macrogenetic level, the person is creating a duality between linguistic and social structures, as langage explicates. Contrary to the microgenetic level at which the person is purely operating within the domain of signs as langue refers to. These are the signs that serve as linkages between thoughts and speaking activity. [33]
While a person goes through the step-by-step process of the microgenetic level, he or she does so by constantly referring to the macrogenetic level. An individual, for example, experiences a pounding headache, which hinders him or her to think or act in a way that person normally is used to acting. He or she asks him/herself whether he or she is o.k. or not, concluding that he or she is not (microgenetic model). Immediately the individual will assess if he or she has felt such a headache before or not (macrogenetic model). And whether the person has or not will then influence his decision in step (3) of the microgenetic model. What can the individual do to make him or herself feel better? While reflecting on what has helped in the past, he or she simultaneously anticipates future emotions and feelings. How will the individual feel when he or she does not take any medication versus when taking medication? How has the person felt in the past when taking this medication? Considering such reflections at the macrogenetic level influences the person while going through an individual process of step-by-step problem solving. The interaction of the reflections from the outside world and the inner step-by-step problem solving mechanisms take place in the same way the interaction of langage and the opposition of langue and parole does. Gathering information from the outside world will influence the internal mechanism accordingly. Depending on how the illness has panned out in the past the person will be either more likely to take the same medication again or will decide to talk to a doctor first. [34]
Thus, while each level serves a different function in the process of making decisions, they are inevitable working in some correspondence to each other. A previous study (JOERCHEL, 2002) has shown that people use specific heuristics in decision-making processes about medication and that these differ from individual to individual. Particularly what kinds of heuristics are being employed did not become evident. Thus, in the present study an effort was made to demonstrate how the two levels operate in persons' self-reports of dealing with falling ill experiences. [35]
A check-off list with a total of 12 illnesses and bodily discomforts was handed to the subject before interviewing them (see Appendix). Before checking off any of the discomforts they have had in the past, the people were asked to mark on the questionnaire their age, gender, year in college, and whether they were taking any medication at the time and if so to specify which kind. The illnesses and bodily discomforts included the stomach flu, back pain, mononucleosis, the cold, ear infection, urinary track infection, fever, asthma, cramps, headaches, giant papillary conjunctivitis, and allergies. At the end of the check-off list the subjects were given the opportunity to check "other" and list any other illness or bodily discomfort they wished to list. For the interviews a tape recorder with a hetero-directional microphone2) was used. [36]
Clark University classes were used to recruit participants. After briefly introducing the research project to the whole class students were asked to write down their e-mail address if interested. Students were contacted and scheduled for interviews until a total of 25 was reached. These 25 students included two males and 23 females. Their ages ranged from 17 to 23. Subjects were not asked about their ethnicity. Even though the sample was taken from an American college population there were some foreigners among them (e.g., a subject from Greece). [37]
Once an interview was scheduled via e-mail the researcher waited for the subject in a testing cubical at Clark University. The checklist was placed on the table for the participants to fill out upon entering the testing cubical. After completing the check list subjects were asked if they had any questions. If they did the researcher would answer them and if not the interview would begin. Questions were asked systematically, starting with the kind of medication the person was taking at the time. They were also asked (if women) whether they took birth control pills or not, and whether they considered them as medication or not. Then the researcher went by the check list and asked about each illness or bodily discomfort marked on the sheet of paper. Subjects were asked various questions in the interview, which were designed to clarify the specific heuristic each individual uses. The interview included questions of what the subject did in various situations of falling ill, then asking them to reflect upon their feelings at the time, questions of how they thought they had come to their chosen conclusion, as well as what family members or friends thought about them being ill and about medication. [38]
Interview included the following questions:
"What do you do when you first get the flu?"
"Do you try and do other preventative actions before taking medication?"
"Why, why not?"
"Can you generalize when you usually take medication?"
"Who told you (if anyone) what to do when you get sick?"
"Why do you take medication for the flu but not for a headache (or vice versa)?"
"Do you consult a doctor before taking medication?"
"How do people in your family treat illnesses?" [39]
Interviews did not take longer than half-an-hour, most ranging between 15 and 25 minutes. At the end of the interview the subject was asked if she/he had any further questions, if so these were answered, and then were thanked for their participation. [40]
All the interviews were read carefully and analyzed according to the two models described above (microgenetic and macrogenetic models) and to common themes. Which level (the macrogenetic or the microgenetic) did the interviewee use to create their individual beliefs about an illness and a medication? How did either belief lead to or guide the behavior of taking medications? Furthermore, was there a common denominator in all the interviews, what key issues repeatedly appeared, and did the interviewees represent these issues in a similar fashion? Special attention was given to how specific interviewees projected overall themes that where found in every interview, such as trust, and work ability. [41]
The data collected ranged widely from persons who were quick to take medications to persons who very rarely took medications. People who reported taking medications very readily had usually not experienced any other discomfort from the actual medication. Individuals who either experienced side effects directly or who saw a friend or a family member suffer from side effects were more reluctant to take medication as soon as they feel a bodily discomfort. Further, persons who had more knowledge about the effects of medication in general were more reluctant to resort to medicines upon falling ill. [42]
4.2 Reasons for taking medicines
From the eight subjects who reported taking medication on a daily basis, the type of medication taken ranged from allergy and acne medication, growth hormones and synthroids for a thyroid disorder, over Adderoll3), to anti depressant and anti psychotic medication. While six subjects marked down on the questionnaire that they took a form of birth-control at the moment, upon asking each individual during the interview, three reported that they were taking birth-control pills or some other version of birth-control, but did not view it as a medication and thus did not say so on the questionnaire. Upon asking about whether birth-control pills are medication or not, 12 females reported that it was medication because either it affected their body chemistry, it was in the form of a pill, or because it interfered with other medication such as antibiotics. Those who did not consider birth-control pills medication usually gave the reason that medicine is a substance that is supposed to cure some illness or discomfort in the body and preventing pregnancy does not belong to this category. [43]
The definition of medication varied as much as the perception of whether birth-control pills are medication or not. What falls under the category of medication, and what doesn't? What does it mean to take something for a discomfort? These are questions all subjects were confronted with and most of them, except for three, felt uneasy about taking medication at all. This uneasiness was accompanied with the notion of medication being poisonous. Even though most subjects agreed upon medicines being poisonous to some degree, the degree varied. While one subject reported stopping the birth-control pills, because it made her uneasy to take a pill every day, another reported taking pain releasers as soon as she felt any sign of a headache, because she did not want to deal with any sort of pain. Yet, usually subjects did not like the idea of always "popping pills" and tried not to take medicine if they did not need to. Upon further questioning why, medicine always took on a negative connotation. While medicine has the power to relieve bad symptoms, the same power can also produce symptoms. Instead of helping the body regain the normal strength, the potential of harming it is always present. [44]
The notion of the body being a working machine, which needs to be maintained at optimal working condition, was present in every interview. Subjects were much more willing to take medication if the illness or the bodily discomfort in one way or another hindered the usual work speed. Most subjects reported some reluctance about taking medication in general and would always rather not take any, while others reported only taking some if they had an exam or a class to go to. [45]
Before interviewing subjects, they were asked to mark off all previous illnesses or discomforts on the list presented to them, which they have experienced in the past (see Appendix). 23 subjects marked off having previously experienced headaches (see Table 1). Interestingly, the only two subjects who did not mark off having headaches were the two males. The whole study included only two males, which unfortunately is not enough to make any conclusion about the difference between males and females. Yet, from these two males, one did not have any illnesses that were listed on the sheet and claimed not to have had any other illness either. The second male had mononucleosis, but not any other illness or bodily discomfort. After the headaches, the most frequent illness experienced by subjects was the cold (22 reported having had the cold). Cramps were reported 21 times, 20 subjects reported having had a fever and the stomach flu and 14 reported having back pain. Ear infections were reported 13 times and allergies 11 times, mononucleosis and urinary track infections were reported 6 times and eye infections 5 (giant papillary conjunctivitis). Only three subjects reported having had asthma. Among the three subjects who marked off having had some other illness, one was a gastrointestinal disorder, one was diarrhea and the third was sinuses. The distribution of each bodily discomfort can be seen in the Table 1, illnesses are listed according to frequency with headaches being the most frequent and asthma and other the least frequent. Yet, in order to fully understand the exact process individuals go through while deciding to take medication, individual analysis is necessary.
|
Subjects Illnesses |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
11 |
12 |
13 |
14 |
15 |
16 |
17 |
18 |
19 |
20 |
21 |
22 |
23 |
24 |
25 |
|
Headaches |
x |
x |
|
|
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
|
Cold |
x |
x |
|
|
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
|
x |
x |
x |
|
Cramps |
x |
x |
|
|
x |
x |
|
x |
x |
x |
x |
|
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
|
Stomach flu |
x |
x |
|
|
|
x |
x |
x |
|
x |
x |
|
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
|
Fever |
x |
x |
|
|
x |
x |
x |
x |
x |
|
x |
|
x |
x |
|
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
|
Back pain |
x |
x |
|
|
|
x |
|
|
x |
|
|
|
x |
|
x |
x |
x |
|
x |
x |
x |
|
x |
x |
x |
|
Eye infection |
|
|
|
|
|
x |
x |
x |
|
|
|
x |
x |
x |
x |
|
x |
x |
x |
|
x |
|
x |
|
x |
|
Allergies |
x |
x |
|
|
x |
|
x |
x |
|
x |
|
|
|
|
|
|
x |
|
x |
|
|
x |
|
x |
x |
|
Mononucleosis |
x |
|
|
x |
|
|
|
|
|
|
|
x |
x |
|
|
|
x |
x |
|
|
|
|
|
|
|
|
Urinary track infection |
|
|
|
|
|
x |
|
x |
x |
|
|
x |
|
|
|
|
|
|
|
|
|
|
x |
|
x |
|
Giant papillary conjunction |
|
|
|
|
|
x |
|
|
|
|
|
|
|
|
|
|
x |
|
x |
|
|
x |
|
|
x |
|
Asthma |
x |
|
|
|
|
|
x |
|
|
|
|
|
|
|
|
|
|
|
|
x |
|
|
|
|
|
|
Other |
x1 |
|
|
|
x2 |
|
|
|
|
|
|
x3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
Table 1: Illnesses mentioned by the participants (Others: 1 = Gastrointestinal disorder, 2 = Diarrhea, 3 = Sinus infections [46]
It is necessary to look at some interviews in detail in order to illustrate some of the issues mentioned above. Two interviews were specifically rich in social as well as individual representations of illnesses and the use of medication and therefore they are discussed in further details here. For convenience, the interviewees are labeled S and the interviewer is labeled I. Particularly interesting aspects of the interviews, highlighted by underlining, are specific representations and the importance of maintaining these representations individually as well as collectively. Reference points for the interviewee's representations (notions from the collective as well as the individual level that help to maintain, further strengthen or simply support already existing concepts about medication) are also underlined. The representations pointed out here necessitate the use, or precisely the lack of use of medication by an interviewee. [47]
4.3 Data analysis subject 23: Myths and memories that guide decision making
Let us consider an example, in which the subject (23) was concerned about getting sick in the future and thus took pre-emptive steps to prevent it. In this case future anticipations were crucial in deciding what actions to take. Upon asking her if she takes any vitamins or any other supplements she replied that she does not on a regular basis but because she knows that her body lacks iron she does take an iron supplement right before, during and after her menstruation.
"S: I take iron, because when you have your period you lose a lot of red blood cells, and I am borderline iron deficient, so I don't ever have any problem with it, but when I get my period you can see it on my face, my eyes get so black. So it's, I start, I usually start like a week before or something like that and then continue a week after that. So you can say I do take vitamins, but not regularly." [48]
While making the decision about taking medication in order to prevent iron insufficiency in her body (operating within the macrogenetic model), she is making personal assessments to future anticipations and reflecting on past memories. She knows that she has iron insufficiency during her menstruation, she has had it in the past, and she does not want to have it again, it makes her tired and her rings underneath her eyes become very black, thus anticipating how she will feel and deciding to take action about it. [49]
A more sufficient example in explicating the influence of future anticipations is where the subject elaborates on how she knew that she needed more vitamins usually when traveling to Alaska.
"I: Do you take anything else like that?
S: But I, no, um, like O.K. if I am going to travel, like when I went to Alaska to do research and I knew I was going to have to do physical work and I am exposed to the cold which I am not used to, well after three years in Massachusetts, but um, I took Echinacea, I do things like that. And the way I use vitamins and like remedies like that is when I feel like I am getting a cold or something, because of school I just boost my system immediately." [50]
Again, here the subject is anticipating certain hardships she will pass through because of temperature change and change of action. Reflecting on how strong her immune system is at the moment, she anticipates her immune system not being able to fight off what it needs to in order to keep the body healthy and thus tries to give her immune system extra strength by using various supplements. [51]
When the subject was asked whether or not she usually takes medication her answer was remarkable because of the clarity of the ambiguity about medication and the internal versus external factors.
"I: O.K. you said a couple of things that I wanted to ask you about, one was, um, you don't usually take medication, why?
S: Well I don't take any, how do you call it like, drugs for any mental reasons, but I, and I usually don't, what I mean by when I say I usually don't take medication is that, I like, because it tires me down, like it is really tough for my system, I only want to use it when I have to, so basically when I get sick and I have fever for example, I'll take medication to bring it down. Now in colds, for colds and things like that I'll take like pain releasers and fever reducers and things like that. If it gets worse I'll go then to the doctor or to somebody who can give me something. Like for example, I was sick a while ago and my tonsils were really irritated and had white spots and everything, so I went to the doctor and the lady was actually really nice, she said you know you can start taking penicillin right now and then when the test come out, um, you either are going to stop or continue doing it, but it seems that it is really irritated and it might end up being really bad, you might want to take the medication now and then stop it, which it's kind of like, it's O.K." [52]
In a normal setting the subject does not want to take medication, having negative feelings about it, because she believes her body cannot properly decompose the substance without doing harm to the body. Notice the poisonous connotation that the medication takes on. Yet, when she feels ill, when she feels as though she needs some medication to regain normal strength, the medicine takes on a positive face and her attitude changes in terms of "wanting to take medication". After asking herself if she is doing fine or not (microgenetic model), she comes to the conclusion, via step 2 of the model (Why not), that she knows what is wrong with her (she has a fever) and in step 3 (What can I do to make me feel better?) decides to take medication. She knows when she has a fever she will take a fever reducer and she knows when she has a cold she will take a pain releaser. [53]
In dealing with the ambiguity of taking medication the subject moves from the use of the microgenetic model eloquently into the macrogenetic model. When the microgenetic model has been completed, she reaches out to other members of her community, in this case the doctor or someone who can give her something. At this point she is not under the impression of being able to handle the situation on her own and is looking for outside support. What will the doctor do? He will give her something that will take away her discomfort: "If it gets worse I'll then go to the doctor or to somebody who can give me something." [54]
It is interesting to see how she justifies her actions. This is very much along the lines of what a previous study conducted by JOERCHEL touched upon. The notion of the body being a machine, which needs to function well so the work can be done, was elaborated before (JOERCHEL, 2002). It is a separation of the body and the feelings. It is not the person who is feeling ill; it is the body that needs to function properly so that the person can do the work. Thus he or she needs to take certain actions they might not approve of in normal circumstances when their body is healthy.
"I: So that is what you did?
S: Yes, so that is what I did. Cause I couldn't afford to miss school and I was in real pain, it wasn't like a soar throat, they were really swollen and they had really big white spots on them, so from the doctor's perspective there was a chance that I had Mononucleosis and this would have been something I would be taking anyways and I know it gets really, um like, it can get really bad for you basically. So I like, sacrificed myself on that and I took the medication even though I ended up not needing it." [55]
The above example is consistent with the subject's ambiguity of taking medication. If she would have been seriously ill, she would have needed the medication and then it would have not been a sacrifice. Yet, because she was anticipating her body to not function in a sufficient manner for her to get her work done at a normal rate, she "sacrificed" herself and took the medication. So while she thinks taking medicines is too tough on her body, she is afraid of future disabilities and thus takes into account the extra work her body needs to do when taking medication. [56]
While asking herself if she is doing fine, and coming to the conclusion that she is not (microgenetic model), she asks what the doctor thinks and anticipating how she will feel in the future (macrogenetic model). [57]
In the next example the subject reflects on how she was raised and what she was taught to do when falling ill.
"I: You have mentioned your mother a couple of times, how is she with medication?
S: Um, she, well my mother had to take a lot of medication, she had um, how do you call it cortisone. So she is the kind of person that knows the upside and downside of taking medication really well, and I would say that she tends to give, because we are away every time we are sick she tries to give us medication and she knows that she raised us in a way that we won't take medication right away. And she knows that we won't take it. So she will always make it available for us, but she is not, she is like for example when I got sick vomiting and all those things she could have taken me to the hospital, and she didn't, she did the whole thing by herself and she spoon-fed me with water so I wouldn't dehydrate and all those things. So I would say she is a very good combination of using both." [58]
Here it becomes clear how the microgenetic model is partially based on the macrogenetic model. The steps that the subject moves through while feeling a bodily discomfort are parallel to what she reports about her mother. As a rule she would rather not take medication because of the "downfalls" of it. Yet, when she is under the impression that her body needs something she will not hesitate to take some medicine. The subject will go through various steps of self diagnosis before asking for professional help, and only if she cannot cure her body herself will she resort to a doctor or a nurse who is able to prescribe her stronger medication. According to the reflections of the subject, the mother presumably would take similar actions. The subject remembers getting sick and instead of being to the hospital, presumably the easier solution, her mother chose to do whatever is in her power to get the subject well on her own. Thus, when the subject falls ill today she will first try to diagnose herself before seeking outside help. While making decisions about what is wrong with her and what to do to make herself feel better, she reflects on how her mother brought her up to act in situations of illness. [59]
Notice how in the following example the subject reflects on broader beliefs that are present in her culture, which she uses to establish her personal meaning system about medication.
"I: Would you ask the doctor for alternative things or alternative mediation?
S: Yes, I would. I would usually. Although if I talk to a doctor I would probably ask for alternative medication more than asking for alternative treatments, because I don't expect him, although some doctors they do say you know, just make a hot tea and you'll be fine. I guess, but um, I also think it is important to mention that most of the doctors that I have been exposed to, they are like Greek doctors, and since I have been in the US I have gone to the Health Center at school, but I haven't really been to any doctors." [60]
The subject has created a personal meaning system through her personal culture about taking medication and particularly the role of a doctor. This personal culture has come out of what people close to her believe (her mother only goes to doctors if she needs to and then she takes the medication that was prescribed to her), and a cultural belief about doctors in general. In her home country, as this subject recollects, "doctors prescribe chemicals, not alternatives," thus when the subject decides to seek professional guidance, she goes under the presumption that the doctor will recommend some medicines instead of remedies. This notion plays an important role in her self diagnosis and her decision about what to do when falling ill, as the following example shows even more clearly.
"S: Yea, I would be more willing to take remedies if she suggests it instead of taking medication. So for medication I'll trust my doctor or my mother, because I know she trusts the doctor and she knows me, she knows what my system can take." [61]
Trust is an important notion in the macrogenetic model. While persons use general social representations, such as that doctors prescribe medicines, not alternative supplements, in the macrogenetic model, each individual will vary in terms of how they will trust, whom they will believe and what their actions will be accordingly. The notion of trust is further elaborated in the next example.
"I: I don't know if that necessarily matters, because I try to figure out if you trust them or not, the doctors that you are seeing. So for example, if a doctor says you should take this medication then you'll take it, but if your roommate comes, or you see it on a shelf, then would you take it.
S: No, no, no, especially when it is medication, like, medication, well if a doctor recommends something, I have to accept that I'll probably take it. I'd like to know about it, so I usually ask, but I won't pose any arguments about it usually. Now I usually ask people about remedies and I am more likely taking like an Echinacea concentrate, a few drops under my tongue if my roommate suggests it, but I will not take any kind of medication if she suggests it." [62]
Here the subject makes a clear distinction between medication, remedies, authoritative figures and friends. While she will trust her mother and her doctor for medical advice, she does not trust her roommate for that. She does trust her roommate on advice about remedies. The subject has separated the two and thus internally justifies her decision of when to take medication and when not. [63]
The above examples portray how a person uses the macrogenetic model as a base for the microgenetic model. The macrogenetic model includes issues like trust, cultural beliefs and future anticipations. But it also includes myths that float around, either in the given society as a whole or in the closer circle. The next example talks about these myths that are created within the subject's family.
"I: Do you think you learned it from her (the mother), the way you handle medication or not?
S: Um, I think I did, um, well the funny thing is that she brought me up telling me a story that when I was a baby I was bulimic and um, which is basically that I would eat a lot, drink a lot of milk, focus all my interest on eating and then throwing it all up. So she took me to the doctor and the doctor suggested medicine and she freaked out. She said I am not giving my baby, my infant you know medicine, and like that they give to old people. So she basically did other things for me. Like every time I would cry for a cookie she would lift me up and tickle me or take me for a walk in the woods or something like that. So I'd say, yea, I learned a lot from her in that sense that she would always try, and my dad too, they would always try and make us, um fight with any kind of problem, especially with diseases, with what we have in our body and then get help. But they never made us think that we have to count on external facts in becoming better." [64]
In this example a myth is kept in the family as an example of what to do when falling ill. It is a representation of how the family deals with medication. While the subject does not remember the instance itself, she only remembers the story of the instance as told by her family and thus has created her own memory from the story. In this sense, a family myth is part of the personal culture. While it refers to what the family believes in, it is made into a personal memory. [65]
It is such memories that persons reflect upon while going through the microgenetic model of decision making about medication. They function as mediating devices within which personal cultures are directed in one way or another (GUPTA & VALSINER, 1996). [66]
4.4 Data analysis subject 2: Ambivalence about taking medication
Another example is Subject 2. This subject was taking allergy medication at the time of the interview and upon asking her whether she consulted a doctor or not her answer had an unsatisfying tone to it.
"I: Did you go to a doctor to ask for it?
S: Ah, I've never been to an allergist, but I've asked doctors and they said just try Benadryl. They really didn't seem to care too much.
I: And they (the doctors) put you on Allegra now?
S: No, I decided to take that by myself, because, like, the Benadryl didn't really work that well and, like, since the doctors didn't seem to care I asked my roommate and she suggested Allegra, so, like, I tried it and it works." [67]
Her reaction to the doctor not caring about her taking allergy medication makes the decision easier for her to take just any allergy medication. At the macrogenetic level the subject got weak feedback from authorities and thus decided at the microgenetic level to take other medication, not that which was suggested by the doctor. [68]
This subject also brought in the notion about her body being a machine. When she was asked why she needed to take any allergy medication she replied that her allergies are so destructive that she cannot function normally without allergy medication.
"I: How did you decide that you needed allergy medication?
S: Well, cause I'm allergic to dust mites, which are everywhere, and I'm living in an old house here, and I'm living with a cigarette, well a cigarette smoker is not in my room, but in my apartment, so that affects me too, and here is a class room that I have that I am very allergic to, and I sneeze all through class, so it disrupts my note taking." [69]
The ambivalence about taking medication at all is very clearly present in this interview. Even though the subject is currently taking allergy medication on an every day basis, she refers to the weariness that medication gives her several times throughout the interview. In this example she stops taking birth-control pills because she does not like "putting hormones" into her body, and yet, immediately after reporting the reluctance about taking medication she reports taking anything that she can keep down when she gets the stomach flu.
"I: Are you on birth control?
S: No, but I did try that for probably four months, maybe, I think four months. That was like, I didn't like taking that every day, it made me nervous 'cause like, I was just afraid that it was going to change like, I don't know, my chemical composition of my body or something.
S: Yea, I just don't like the idea of putting hormones into me, and I don't like taking so many pills. So I kind of got off that.
I: And when you had the stomach flu, how was that? Did you take medication with that? It's probably hard to keep anything in your stomach when you have it.
S: Yea, the stomach flu, I'm really sick when I have the stomach flu. When I have the stomach flu, I beg my mother to shoot me (laugh). I get really bad, I mean I don't, I think everyone gets it really bad, but like I feel like it is the end of the world when I get it. So as long as I can keep something in me I'll take anything. I forgot what, I'm not even conscious when I am sick, I like, whatever I can get and keep in my body ..." [70]
The notion of not wanting to take a hormone into the body relates to the notion of medication being poisonous. While it is clear that there are benefits (not getting pregnant, reducing cramps, regulating the periodic cycle), there is also something bad about it. In this case the subject does not know exactly what it is; yet, the feeling is strong enough for her to decide to stop taking birth control pills. [71]
The ambivalence of taking medication is immediately eradicated at the microgenetic level. While the subject clearly does not approve of taking medication, she internally justifies taking medication when she is sick. It is okay to take medication for the stomach flu because then she feels so bad that "she thinks she is dying." Once the subject is in a state of distress because of an illness, her negative conception of medication at the macrogenetic level becomes positive at the microgenetic level. [72]
A similar contradiction occurred when the subject was asked about considering alternatives to medication:
“I: Do you ever think of, so you consider alternatives, or try them out before taking medication?
S: Yea. I always do before taking medication, I like to make sure that I am hydrated enough. Um, or that, you know, that I have been eating a well balanced, so that I have enough vitamins in my diet and minerals. Um, and if like, you know if I'm pretty sure I am sick, you know, like my whole family is sick, then I'll take something.
I: What about cramps? Do you get them on a regular basis?
S: Yea, yes, I load up on ibuprofen. Not really load up, I'll take like two or three at a time." [73]
As with the above example, the subject makes it clear that she does not like taking medication and yet, she does not hesitate to "load up" on Ibuprofen when she gets cramps. But, as the interview goes on, she does not change her position about being reluctant about taking medication.
"I: How come there are only a few (medicines) that you take?
S: 'Cause I really like to limit it, I like to keep it to a minimum what I am putting in my body.
I: Why is that?
S: It makes me nervous. I don't like mixing, I don't like trying to make myself, I, I know I don't think I can become dependant on anything, especially like, cause I don't take it that often, but I don't think it's really necessary to put stuff in my body when it is not necessary." [74]
What does it mean to be sick? When deciding whether to take medication or not, a person first has to have a notion of being sick. GADAMER (1993) has discussed this issue in detail and come to the conclusion that a "healthy" person is one who is filled with energy and joy and who forgets about the hardships that the body goes through everyday. While such persons might not constantly think about themselves as being healthy, the fact that they are not thinking about aches and discomforts is enough for a person to be healthy (GADAMER, 1993). [75]
But what happens once a person does feel discomforts and aches? Some get some rest, some seek professional guidance and others resort to medication. This paper discusses the precise moment of persons deciding to take medication. The range of illnesses is high and thus the wide range of medications. Further, each culture and even within each culture, the nature of when and which medication to use varies as well. Yet, as GOLDMAN, PEBELY, and GRAGNOLATI have pointed out, the symptoms associated with the illness, their perceived severity and the belief about the causes are important determinants to what kind of treatment is actually sought (GOLDMAN, PEBELY, & GRAGNOLATI, 2002). Besides discussing the determining factors of what kind of treatment, and whether to take medication or not, the risk factor of a specific treatment or medication needs to be addressed as well. HEYMAN has discussed this issue in the context of the notion of risk escalators (HEYMAN, 2004a, 2004b). Creating health care risk escalator models, such as HEYMAN has discussed and as subjects did when discussing their likelihood of taking medication when side effects were less likely to occur, is helpful in understanding how a person balances risks. Furthermore, it undermines the certainty of undesired consequences arising from an intervention against the risk of harm occurring if an appropriate powerful preventative strategy is not adopted. The two models presented in this paper are necessary to combine all relevant factors that are determinants in the problem of making a decision about medication—such as the severity of symptoms, the beliefs about them, and the risk associated with not seeking a preventative or healing strategy. [76]
The two models explicated above are designed to analyze the data collected in this study appropriately. Yet, the model can be applied to any person in the process of making a decision to take medication. While each person has an individual process which differs every time the person is confronted with a new illness, every individual will go through a microgenetic process that is coordinated with reflections on the macrogenetic level. Cultural beliefs, personal memories and future anticipations are brought into their decision making by people at the macrogenetic level. Persons view the world from very different perspectives according to the location and time (MOREMAN, 2002). The macrogenetic model represents these universal differences, while the microgenetic level of analysis helps with the inner personal model of deciding whether to take medication or not. Personal assessments of what is wrong with the body and what needs to be done in order to regain optimal health are analyzed with the help of the microgenetic model. [77]
The microgenetic model is described separately from the macrogenetic model, yet, the interactions between the two are crucial. As the threefold analytic scheme of langage, langue, and parole shows, a person facing the problem of making a decision is in dialog with external entities and internal thoughts and memories. In the threefold analytical scheme this dialog refers to linguistic processes within and outside of a person. The dialog between the macrogenetic and the microgenetic model does not necessarily occur linguistically. The relation of the microgenetic and macrogenetic model is a dialog of representational signs. While an individual is operating at the microgenetic level, inferences to the macrogenetic level are constantly made. The various steps that individuals go through depend very much on the collective culture, the individual culture and various beliefs held by the person. These notions are represented in our macrogenetic model. While humans in every culture share certain main features such as caring for family members, providing food for loved ones and taking care of the sick ones in community, how specifically this is done varies tremendously (MOREMAN, 2002). Cross-cultural differences are seen in all behaviors of humans, also in what kind of treatment will be sought upon falling ill. But cross-cultural differences are not the only ones. There are differences within each culture as well as within each neighborhood. Differences can even be found within the same family. Similarities in the overall culture operate within the macrogenetic model. What sorts of myths are being carried on? Which overall beliefs are held? Subject 23 clearly presents the belief held culturally that doctors do not prescribe alternative actions to medication; they are there to help a person when feeling ill with medicines. Further on she describes very nicely a myth carried on within her family about herself being bulimic when she was a baby and the reaction her mother had to the doctor suggesting medication. [78]
The view of the body being a machine is a further widely held belief that is discussed in this paper. A person will make a very different decision if the idea is to keep it running in order to work, than when the notion is focused on staying fit for health purposes (HERZLICH, & PIERRET, 1987). JOERCHEL (2002) elaborated this idea and concluded that a person is much more likely to take medicine if the illness affects the work this person has to do, than when it is not affected. An ongoing theme, which has persisted in this study as well, was the willingness to take medication when the illness, or simply a discomfort, distracted the person from performing regular tasks such as work or school. Subject 2 decided to take allergy medication because it disrupts her daily activities such as note-taking, hindering her to function normally. The macrogenetic level of analysis incorporates any kind of belief or myth held by individuals that function as reference points for the microgenetic level. [79]
Cultural beliefs are maintained throughout the decision-making process. After assessing how a person at that moment feels, decisions whether medication is the appropriate solution for the problem will depend on these cultural beliefs. But emotions and personal feelings play a crucial role as well. The microgenetic model allows for analysis on such an inner personal level. How does the person actually feel? What is wrong? What is the best solution from all the options that are present? While each model individually is important in describing the process of taking medication, they work together and one alone will not be sufficient for explicating the problem of making a decision on whether to take medication or not. [80]
A study on the decision-making about medication
Please fill out the form below regarding general information about you and indicate with a check mark, which of the illnesses/bodily discomforts listed below you have suffered in the past.
General Information:
Age:_______
Sex:_______
Year in College:_________
Who do you live with (family, friends, room-mate, etc.):______________
Do you take any medication at the moment? (If yes, what kind?):______
________________________________________________________
Illnesses and Bodily Discomforts:
___ Stomach Flu
___ Back Pain
___ Mononucleosis
___ Cold
___ Ear infection
___ Urinary track infection
___ Fever
___ Asthma
___ Cramps
___ Head-aches
___ Giant papillary conjunctivitis
___ Allergies
___ Other:_________________
1) An American brand name for a pain reliever, equivalent to Aspirin. <back>
2) A microphone that picks up both the interviewers and the subjects voice, while filtering out most of the background noise. <back>
3) A drug for attention deficit disorders. <back>
Abbey, Emily & Valsiner, Jaan (2003). Emergence of meanings through ambivalence. Paper presented at the Symposium Meaning construction: Language, metacommunication and culture (A.U. Branco & C. Sinha, conveners) at the European Conference on Developmental Psychology, Milano, August 28.Gadamer, Hans-Georg (1993). Ueber die Verborgenheit der Gesundheit. Frankfurt am Main. Suhrkamp.
Gigerenzer, Gerd; Todd, Peter M. & the ABC Group (1999). Simple heuristics that make us smart. New York: Oxford University Press.
Gigerenzer, Gerd & Kurzenhaeuser, Stephanie (2004/in press). Fast and frugal heuristics in medical decision making. In Roger Bibace, Jim Laird, Kenneth Noller, & Jaan Valsiner (Eds.), Science and medicine in dialogue . Westport, Ct.: Greenwood.
Goldman, Noreen; Pebley, Anne R. & Gragnolati, Michele (2002). Choices about treatment for ARI and diarrhea in rural Guatemala. Social Science & Medicine, 55, 1693-1712.
Gupta, Sumedha & Valsiner, Jaan (1996). Myths in the hearts: Implicit suggestions in the story. Paper presented at the Second Conference on Socio-Cultural Studies, Geneva, September 14.
Herzlich, Claudine & Pierret, Janine (1987). Illness and self in society. Baltimore, Maryland: John Hopkins University Press.
Heyman, Bob (2004a/in press). A qualitative approach to health risks. In Roger Bibace, Jim Laird, Kenneth Noller, & Jaan Valsiner (Eds.), Science and medicine in dialogue. Westport, Ct.: Greenwood.
Heyman, Bob (2004b/in press). Health risk escalators. In Roger Bibace, Jim Laird, Kenneth Noller, & Jaan Valsiner (Eds.), Science and medicine in dialogue . Westport, Ct.: Greenwood.
Joerchel, Amrei (2002). Falling Ill and the use of medication: An analysis of personal cultures. Presented at the 12th Annual Academic Spree Day, Clark University. Worcester, MA.
Mellers, Barbara A.; Erev, Ido; Fessler, Daniel M.T.; Hemelrijk, Charlotte K.; Hertwig, Ralph; Laland, Kevin N.; Scherer, Klaus R.; Seeley, Thomas D.; Selten, Reinhard & Tetlock, Philip E. (2001). Group report: Effects on emotions and social processes on bounded rationality. In Gerd Gigerenzer & Reinhard Selten (Eds), Bounded Rationality: The Adaptive Toolbox (pp.263-279). Cambridge, Ma.: MIT Press.
Moerman, Daniel E. (2002). Meaning, medicine and the "placebo effect". Cambridge, UK: Cambridge University Press.
Simon, Herbert Alexander (1982). Heuristic problem solving: the next advance in operations research. In Herbert Alexander Simon, Models of bounded rationality: Economic analysis and public policy (Vol. 1) (pp.380-389). Cambridge, Ma.: MIT Press.
Valsiner, Jaan (1997). Culture and the development of children's action (2nd ed.). New York: Wiley
Valsiner, Jaan (1998). The guided mind: A sociogenetic approach to personality. Cambridge, Ma.: Harvard University Press.
Valsiner, Jaan (2001). Process structure of semiotic mediation in human development. Human Development, 44, 84-97.
Amrei C. JOERCHEL, Social Psychology student in the MSc Program at London School of Political and Economic Sciences
Contact:
Amrei C. Joerchel
G 7, 11
D-68159 Mannheim,
Germany
E-mail: amreijoerchel@hotmail.com
Jaan VALSINER, Professor and Chair of the Frances L. Hiatt School of Psychology, Clark University
Contact:
Jaan Valsiner
Clark University
950 Main st.
Worcester,
MA 01601, USA
E-mail: jvalsiner@clarku.edu
Joerchel, Amrei C. & Valsiner, Jaan (2003). Making Decisions About Taking Medicines: A Social Coordination Process [80 paragraphs]. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research, 5(1), Art. 17, http://nbn-resolving.de/urn:nbn:de:0114-fqs0401171.
Revised 6/2008